13.3
Impact Factor
Theranostics 2017; 7(1):117-131. doi:10.7150/thno.17031 This issue Cite
Research Paper
Pre-vascularization Enhances Therapeutic Effects of Human Mesenchymal Stem Cell Sheets in Full Thickness Skin Wound Repair
1. Department of Burns, First Affiliated Hospital of Sun Yat-sen University, Guangzhou, China
2. Department of Pathology, First Affiliated Hospital of Sun Yat-sen University, Guangzhou, China
3. Department of Biomedical Engineering, Michigan Technological University, Houghton, Michigan, USA.
# Equal contribution
Abstract
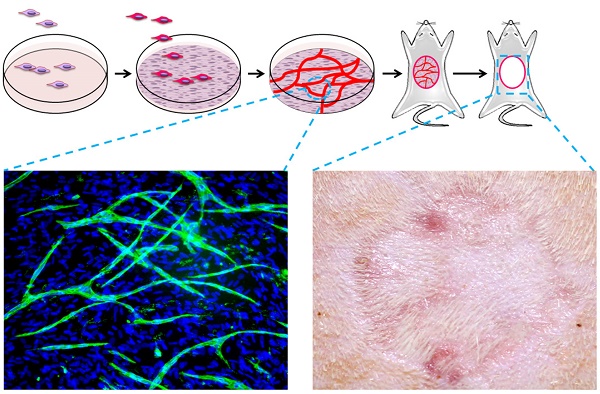
Split thickness skin graft (STSG) implantation is one of the standard therapies for full thickness wound repair when full thickness autologous skin grafts (FTG) or skin flap transplants are inapplicable. Combined transplantation of STSG with dermal substitute could enhance its therapeutic effects but the results remain unsatisfactory due to insufficient blood supply at early stages, which causes graft necrosis and fibrosis. Human mesenchymal stem cell (hMSC) sheets are capable of accelerating the wound healing process. We hypothesized that pre-vascularized hMSC sheets would further improve regeneration by providing more versatile angiogenic factors and pre-formed microvessels. In this work, in vitro cultured hMSC cell sheets (HCS) and pre-vascularized hMSC cell sheets (PHCS) were implanted in a rat full thickness skin wound model covered with an autologous STSG. Results demonstrated that the HCS and the PHCS implantations significantly reduced skin contraction and improved cosmetic appearance relative to the STSG control group. The PHCS group experienced the least hemorrhage and necrosis, and lowest inflammatory cell infiltration. It also induced the highest neovascularization in early stages, which established a robust blood micro-circulation to support grafts survival and tissue regeneration. Moreover, the PHCS grafts preserved the largest amount of skin appendages, including hair follicles and sebaceous glands, and developed the smallest epidermal thickness. The superior therapeutic effects seen in PHCS groups were attributed to the elevated presence of growth factors and cytokines in the pre-vascularized cell sheet, which exerted a beneficial paracrine signaling during wound repair. Hence, the strategy of combining STSG with PHCS implantation appears to be a promising approach in regenerative treatment of full thickness skin wounds.
Keywords: skin graft, human mesenchymal stem cell, prevascularized cell sheet, angiogenic growth factors
 Global reach, higher impact
Global reach, higher impact