13.3
Impact Factor
Theranostics 2020; 10(12):5578-5580. doi:10.7150/thno.46489 This issue Cite
Editorial
Toward clinical understanding of aristolochic acid upper-tract urothelial carcinoma
1. Duke-NUS Centre for Computational Biology,Duke-NUS Medical School, 8 College Road, 169857 Singapore
2. Signature Research Programme in Cancer & Stem Cell Biology, Duke-NUS Medical School, 8 College Road, 169857 Singapore
3. SingHealth Duke-NUS Institute of Precision Medicine, 5 Hospital Drive 169609 Singapore
4. SingHealth Duke-NUS Global Health Institute, 8 College Road, 169857 Singapore
Received 2020-3-30; Accepted 2020-4-13; Published 2020-4-21
Abstract
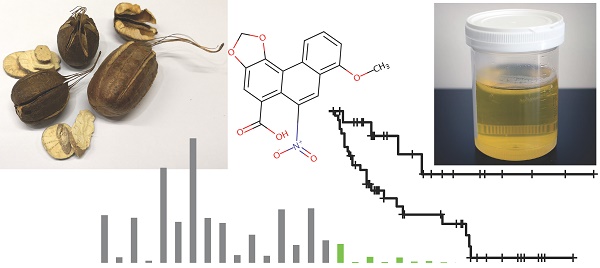
A cluster of patients poisoned by herbal medicine in the 1990s revealed that aristolochic acid (AA) causes kidney failure and upper tract urothelial carcinoma (UTUC). Recent research demonstrated that this was not an isolated incident; on the contrary, AA exposure is widespread in East Asia. This editorial highlights research by Lu and colleagues that investigates clinical characteristics of AA and non-AA UTUCs from 90 patients in Beijing based on the AA mutational signature. The study also detected AA mutations in non-tumor tissue of AA exposed patients and showed that AA mutations can be detected in urine, which might form the basis for non-invasive tests for AA exposure.
Follow up of patients from a herbal-medicine-poisoning cluster in a Belgian weight-loss clinic revealed that aristolochic acid (AA) exposure often causes upper tract urothelial carcinomas (UTUCs) - cancers in the ureter or renal pelvis [1, 2]. Nevertheless, despite concerns that AA exposure might be widespread [3, 4], until recently, AA-induced cancers were studied mainly in two geographic hot spots - the Balkans and Taiwan [5-14]. In the last few years, however, research using AA's DNA-damage footprint - its mutational signature - revealed widespread AA exposure in East Asia [8, 15-20]. Furthermore, mutational signatures also implicated AA in cancer types in addition to UTUC: cancers of the kidney, bladder, bile duct, and liver.
Because these discoveries are recent, as yet there has been little study of the clinical characteristics or of the epidemiology of AA cancers; this includes AA UTUC, even though this was the first type of cancer linked to AA exposure. The study by Lu and colleagues, being the first study based on the AA mutational signature, marks an important step forward in this area [21].
Lu and colleagues reported that 62 of the 90 patients studied have the AA mutational signature. This number seems approximately correct; a more conservative estimate is that 59 patients were exposed to AA (mSigAct signature presence test and Benjamini-Hochberg false discovery rate < 0.05) [15]. The “AA Sig Subtype” tumors in Figure 1A of [21] do not include all AA-mutagenized tumors, because some tumors with clear AA mutations nevertheless clustered away from the tumors dominated by AA (e.g. tumor T013). Nevertheless, the AA Sig Subtype classification provides a reasonable dichotomization between tumors with high AA exposures and those with low or no AA exposure.
Lu and colleagues' data allow a rough estimate of the overall prevalence of AA exposure, even though the study deliberately enriched for patients with self-reported AA exposure. Over all the data (Supplemental Figure S1 in [21]), ~11.5% of the patients reported AA exposure. Using the conservative estimates of AA exposure (not only the AA Sig Subtype tumors) 23 / 27 patients with self-reported exposure had the AA signature, and 36 / 63 patients with no reported exposure had the signature (Supplementary Files 1 and 2 in [21]). We can estimate prevalence of even a low level of AA exposure in this population as (23 / 27) x 11.5 % + (36 / 63) x 88.5% = 60%. The discordance between self-reported exposure and presence of the mutational signature is to be expected. It stems from the bewildering variety of herbal formulations, the frequency of misidentification of herbs, the varying mutagenicity of different AA-related compounds, and the widely varying concentrations of AA-related compounds in different samples of the same herb [22-26]. In contrast to previous studies, assessing exposure by the AA mutational signature is a strength of the paper by Lu and colleagues.
Lu and colleagues observed correlations between the AA Sig Subtype and several clinical factors. The AA Sig Subtype was strongly associated with worse kidney function, which is consistent with the known association of AA exposure with both kidney failure and UTUC. The AA Sig Subtype was also more prevalent in women, in patients with multifocal tumors, in tumors of the renal pelvis as opposed to the ureter, and in tumors of lower stage. Many, but not all of these findings were consistent with previous results that were not based on the AA mutational signature [11, 27, 28].
Notably, Lu and colleagues reported that the AA Sig Subtype tumors had better survival, a finding previously reported by Zhong and colleagues, but not by two earlier studies [11, 27, 28]. Multivariate analysis of Lu and colleagues' data indicates that this is primarily due to the association of AA Sig Subtype tumors with lower tumor stage. To our knowledge, the reason that AA exposure is associated with lower tumor stage has not been studied.
Lu and colleagues also found that the AA Sig Subtype tumors had high numbers of in-silico-predicted neoantigens, and thus might be promising candidates for immunotherapy. Supporting this, AA Sig Subtype tumors had higher levels of infiltrating immune cells. The study also provided extensive confirmation that the AA mutational signature can be detected in non-malignant urothelial tissues [29].
Importantly, Lu and colleagues showed that the AA mutational signature can be detected in cell-free DNA in urine. Given that AA exposure is widespread, noninvasive tests for AA exposure would be highly useful. First, noninvasive tests could be used to study the epidemiology of AA associated cancers, since, as Lu and colleagues' study confirms, it is difficult to estimate AA exposure from retrospective histories. Second, noninvasive tests might also be useful for the clinical management of AA cancers. Third, the tests might be useful for the clinical management of AA exposed individuals, for whom testing positive for AA-exposure might be an indication for regular screening for AA-associated diseases such as kidney failure and cancers of the urinary tract, liver and bile-duct.
In summary, to our knowledge, this is the first study to investigate the clinical characteristics of AA UTUCs using AA exposure assessed by the AA mutational signature. Further studies of the clinical characteristics of AA cancers (UTUC and other cancer types as well) and of the epidemiology of AA exposure should be performed. In particular, the reason that AA UTUCs tend to have lower tumor stage needs to be investigated. Finally, a noninvasive test to detect AA mutagenesis and thereby more accurately assess previous exposure would be a large advance. Consequently, the promising finding that the AA signature can be detected in urine needs to be pursued with the aim of developing a test to detect the presence and level of AA mutations -- one that would be usable in terms of cost, robustness, sensitivity, and positive predictive value.
Abbreviations
AA: aristolochic acid; UTUC: upper tract urothelial carcinoma.
Acknowledgements
This work was supported by the Singapore National Medical Research Council grant MOH-000032/MOH-CIRG18may-0004 and by the Singapore Ministry of Health via the Duke-NUS Signature Research Programmes (funds to S.G.R).
ORCID: AB: 0000-0002-7717-7416; NJ: 0000-0003-4974-2753; SGR: 0000-0002-4288-0056.
Competing Interests
The authors have declared that no competing interest exists.
References
1. Vanherweghem J-L, Tielemans C, Abramowicz D, Depierreux M, Vanhaelen-Fastre R, Vanhaelen M. et al. Rapidly progressive interstitial renal fibrosis in young women: association with slimming regimen including Chinese herbs. Lancet. 1993;341:387-91
2. Nortier JL, Martinez M-CM, Schmeiser HH, Arlt VM, Bieler CA, Petein M. et al. Urothelial carcinoma associated with the use of a Chinese herb (Aristolochia fangchi). N Engl J Med. 2000;342:1686-92
3. Debelle FD, Vanherweghem JL, Nortier JL. Aristolochic acid nephropathy: a worldwide problem. Kidney Int. 2008;74:158-69
4. Grollman AP. Aristolochic acid nephropathy: Harbinger of a global iatrogenic disease. Environ Mol Mutagen. 2013;54:1-7
5. Lai M-N, Wang S-M, Chen P-C, Chen Y-Y, Wang J-D. Population-based case-control study of Chinese herbal products containing aristolochic acid and urinary tract cancer risk. J Natl Cancer Inst. 2010;102:179-86
6. Hoang ML, Chen CH, Chen PC, Roberts NJ, Dickman KG, Yun BH. et al. Aristolochic acid in the etiology of renal cell carcinoma. Cancer Epidemiol Biomarkers Prev. 2016;25:1600-8
7. Hoang ML, Chen CH, Sidorenko VS, He J, Dickman KG, Yun BH. et al. Mutational signature of aristolochic acid exposure as revealed by whole-exome sequencing. Sci Transl Med. 2013;5:197ra02
8. Poon SL, Huang MN, Yang C, McPherson JR, Yu W, Heng HL. et al. Mutation signatures implicate aristolochic acid in bladder cancer development. Genome Med. 2015;7:38
9. Poon SL, Pang ST, McPherson JR, Yu W, Huang KK, Guan P. et al. Genome-wide mutational signatures of aristolochic acid and its application as a screening tool. Sci Transl Med. 2013;5:197ra01
10. Chen CH, Dickman KG, Moriya M, Zavadil J, Sidorenko VS, Edwards KL. et al. Aristolochic acid-associated urothelial cancer in Taiwan. Proc Natl Acad Sci U S A. 2012;109:8241-6
11. Chen CH, Dickman KG, Huang CY, Moriya M, Shun CT, Tai HC. et al. Aristolochic acid-induced upper tract urothelial carcinoma in Taiwan: Clinical characteristics and outcomes. Int J Cancer. 2013;133:14-20
12. Scelo G, Riazalhosseini Y, Greger L, Letourneau L, Gonzàlez-Porta M, Wozniak MB. et al. Variation in genomic landscape of clear cell renal cell carcinoma across Europe. Nat Commun. 2014 5
13. Jelaković B, Castells X, Tomić K, Ardin M, Karanović S, Zavadil J. Renal cell carcinomas of chronic kidney disease patients harbor the mutational signature of carcinogenic aristolochic acid. Int J Cancer. 2015;136:2967-72
14. Grollman AP, Shibutani S, Moriya M, Miller F, Wu L, Moll U. et al. Aristolochic acid and the etiology of endemic (Balkan) nephropathy. Proc Natl Acad Sci U S A. 2007;104:12129-34
15. Ng AWT, Poon SL, Huang MN, Lim JQ, Boot A, Yu W. et al. Aristolochic acids and their derivatives are widely implicated in liver cancers in Taiwan and throughout Asia. Sci Transl Med. 2017 9
16. Zhang W, He H, Zang M, Wu Q, Zhao H, Lu LL. et al. Genetic features of aflatoxin-associated hepatocellular carcinoma. Gastroenterology. 2017;153:249-62 e2
17. Jusakul A, Cutcutache I, Yong CH, Lim JQ, Huang MN, Padmanabhan N. et al. Whole-genome and epigenomic landscapes of etiologically distinct subtypes of cholangiocarcinoma. Cancer Discov. 2017;7:1116-35
18. Zou S, Li J, Zhou H, Frech C, Jiang X, Chu JS. et al. Mutational landscape of intrahepatic cholangiocarcinoma. Nature Commun. 2014
19. Wang X-M, Lu Y, Song Y-M, Dong J, Li R-Y, Wang G-L. et al. Integrative genomic study of Chinese clear cell renal cell carcinoma reveals features associated with thrombus. Nature Commun. 2020;11:739
20. Xue R, Chen L, Zhang C, Fujita M, Li R, Yan S-M. et al. Genomic and transcriptomic profiling of combined hepatocellular and intrahepatic cholangiocarcinoma reveals distinct molecular subtypes. Cancer Cell. 2019;35:932-47 e8
21. Lu H, Liang Y, Guan B, Shi Y, Gong Y, Li J. et al. Aristolochic acid mutational signature defines the low-risk subtype in upper tract urothelial carcinoma. Theranostics. 2020;10:4323-33
22. Michl J, Bello O, Kite GC, Simmonds MS, Heinrich M. Medicinally used Asarum species: high-resolution LC-MS analysis of the aristolochic acid analogues and in vitro toxicity screening in HK-2 cells. Front Pharmacol. 2017;8:215
23. Michl J, Kite GC, Wanke S, Zierau O, Vollmer G, Neinhuis C. et al. LC-MS-and 1H NMR-based metabolomic analysis and in vitro toxicological assessment of 43 Aristolochia species. J Nat Prod (Gorakhpur). 2015;79:30-7
24. Martena MJ, van der Wielen JC, van de Laak LF, Konings EJ, de Groot HN, Rietjens IM. Enforcement of the ban on aristolochic acids in Chinese traditional herbal preparations on the Dutch market. Anal Bioanal Chem. 2007;389:263-75
25. Zhao Z, Yuen JP, Wu J, Yu T, Huang W. A systematic study on confused species of Chinese materia medica in the Hong Kong market. Ann Acad Med Singapore. 2006;35:764-9
26. Kucab JE, Zou X, Morganella S, Joel M, Nanda AS, Nagy E. et al. A compendium of mutational signatures of environmental agents. Cell. 2019;177:821-36 e16
27. Zhong W, Zhang L, Ma J, Shao S, Lin R, Li X. et al. Impact of aristolochic acid exposure on oncologic outcomes of upper tract urothelial carcinoma after radical nephroureterectomy. Onco Targets Ther. 2017;10:5775
28. Cukuranovic R, Ignjatovic I, Visnjic M, Velickovic LJ, Petrovic B, Potic M. et al. Characteristics of upper urothelial carcinoma in an area of Balkan endemic nephropathy in South Serbia. A fifty-year retrospective study. Tumori. 2010;96:674-9
29. Du Y, Li R, Chen Z, Wang X, Xu T, Bai F. Mutagenic factors and complex clonal relationship of multifocal urothelial cell carcinoma. Eur Urol. 2017;71:841-3
Author contact
![]() Corresponding author: steverozencom
Corresponding author: steverozencom
 Global reach, higher impact
Global reach, higher impact