13.3
Impact Factor
Theranostics 2021; 11(10):4585-4598. doi:10.7150/thno.56539 This issue Cite
Research Paper
Mutational spectrum and precision oncology for biliary tract carcinoma
1. Department of Liver Surgery, Chinese Academy of Medical Sciences and Peking Union Medical College (CAMS & PUMC), Peking Union Medical College Hospital, No. 1 Shuaifuyuan, Wangfujing, Beijing 100730, China.
2. Pancreas Center, The First Affiliated Hospital of Nanjing Medical University; Pancreas Institute, Nanjing Medical University, Nanjing 210000, China.
3. Institute of Basic Medical Sciences (IBMS), Chinese Academy of Medical Sciences & Peking Union Medical College (CAMS & PUMC), Beijing 100730, China.
4. Multidisciplinary Molecular Tumor Board of Hepatobiliary Tumors (Departments of Liver Surgery, Medical Oncology, Radiology, Radiotherapy and Nuclear Medicine), Peking Union Medical College Hospital, No. 1 Shuaifuyuan, Wangfujing, Beijing, China.
5. School of Mathematical Sciences, Peking University, Beijing 100871, China.
6. Department of Gastrointestinal Surgery, Peking University Cancer Hospital & Institute, Beijing 100142, China.
7. OrigiMed Co. Ltd, Shanghai 201114, China.
8. Institute of Infectious Diseases, Beijing Ditan Hospital, Capital Medical University, Beijing; Genecast Precision Medicine Technology Institute, Beijing 100089, China.
#These authors contributed equally to this work.
Abstract
Background: The genomic spectrum of biliary tract carcinoma (BTC) has been characterized and is associated with distinct anatomic and etiologic subtypes, yet limited studies have linked genomic alterations with personalized therapies in BTC patients.
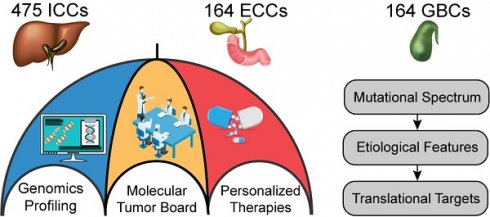
Methods: This study analyzed 803 patients with BTC:164 with gallbladder cancer, 475 with intrahepatic cholangiocarcinoma (ICC) and 164 with extrahepatic cholangiocarcinoma. We determined genomic alterations, mutational signatures related to etiology and histopathology and prognostic biomarkers. Personalized targeted therapies for patients harboring potentially actionable targets (PATs) were investigated.
Results: The median tumor mutation burden (TMB) was 1.23 Mut/Mb, with 4.1% of patients having hypermutated BTCs. Unlike the results obtained from the Western population, the most frequently altered cancer-related genes in our cohort included TP53 (53%), KRAS (26%), ARID1A (18%), LRP1B (14%) and CDKN2A (14%). Germline mutations occurred mostly in DNA damage repair genes. Notably, 35.8% of the ICCs harbored aristolochic acid related signatures and an elevated TMB. TP53 and KRAS mutations and amplified 7q31.2 were demonstrated to negatively affect patient prognosis. Moreover, 19 genes were proposed to be PATs in BTCs, with 25.4% of patients harboring these PATs. Forty-six patients received PAT-matched targeted therapies, achieving a 26.1% objective response rate; the median progression-free survival (PFS) was 5.0 months, with 56.8% of patients obtaining PFS benefits.
Conclusions: Extensive genomic diversity and heterogeneity were observed among BTC patients, with contributions according to potential etiology exposures, anatomical subtypes and clinicopathological characteristics. We also demonstrated that patients with refractory BTCs who have PATs can derive considerable benefit from receiving a matched therapy, initiating further prospective clinical trials guided by molecular profiling among this aggressive cancer.
Keywords: biliary tract cancer, precision medicine, targeted therapy, genomic alterations, molecular screening
 Global reach, higher impact
Global reach, higher impact