13.3
Impact Factor
Theranostics 2026; 16(5):2170-2191. doi:10.7150/thno.124358 This issue Cite
Review
Searching for a HIV-1 Cure
Department of Pharmacology and Experimental Neuroscience, University of Nebraska Medical Center, Omaha, NE, USA 68198-5880.
# Equal contributions.
Received 2025-8-28; Accepted 2025-11-6; Published 2026-1-1
Abstract
Advances in stem cell transplantation, broadly neutralizing antibodies, ultra-long-acting antiretroviral drugs, therapeutic vaccines, cell engineering, gene therapy, and immune-based molecular therapies have highlighted efforts to cure human immunodeficiency virus type 1 (HIV-1). However, none of these are durable. The challenges to achieve complete viral eradication include durability, accessibility, delivery, off-target effects, and practicality. All approaches, including combinatorial therapies with ultra-long-acting antiretrovirals, broadly neutralizing antibodies, or latency-reversing agents, which reduce reservoir size and achieve durable viral suppression, are discussed. These include key translational insights for clinical relevance. Among these, gene-editing technologies have shown promise in disrupting proviral DNA and delivering targeted therapies by targeting latent reservoirs and host viral receptors. This review examines the scientific, clinical, and ethical considerations, focusing on direct viral excision and co-receptor editing as key strategies for a viral cure.
Keywords: CRISPR, CRISPR-Cas9, CCR5, CXCR4, CD4, Gene Delivery, HIV-1 suppression, Viral resistance, Combination antiretroviral therapy, HIV-1 replication
1. Introduction
1.1 Insights of historical relevance from HIV-1 discovery to the present day
Human immunodeficiency virus type 1 (HIV-1) infection causes acquired immunodeficiency syndrome (AIDS). AIDS was first recognized in the early 1980s as a life-threatening condition that primarily affects men who have sex with other men [1]. The syndrome is characterized by the rapid onset of opportunistic infections, such as Pneumocystis pneumonia, and rare cancers, such as Kaposi's sarcoma. In 1983, scientists at the Pasteur Institute, led by Drs. Luc Montagnier and Françoise Barré-Sinoussi isolated a retrovirus from the lymph node biopsies of an individual with AIDS [2]. This virus was first identified as the lymphadenopathy-associated virus (LAV) and human T-lymphotropic virus type III (HTLV-III), both of which selectively target CD4+ T cells. In 1984, Dr. Robert Gallo and colleagues at the US National Institutes of Health (NIH) confirmed that the isolated virus was responsible for AIDS [3]. Subsequent studies elucidated the virus structure, function, and genetic composition and renamed it HIV-1. This discovery marked a significant milestone in establishing the cause of the disease, facilitating successful diagnosis, and ultimately leading to effective antiretroviral (ARV) drug treatment [4]. From 1984 to 1986, recombinant viral clones were ultimately created, leading to the creation of full-length molecular clones of HIV-1 [5-7]. Molecular and biochemical analyses have confirmed that HIV-1 has nine key genes in the viral RNA gene sequence that are associated with the regulation of replication, control, and structural modulation during its life cycle [8, 9].
The principal structural genes of HIV-1 are gag, pol, and env. The gag gene encodes the core p24 (viral capsid) and p17 (matrix) proteins. The pol gene encodes viral enzymes, all of which are essential for completing the viral replication cycle, including reverse transcriptase, viral integrase, and protease. The env gene encodes the gp160 envelope glycoprotein, which is cleaved into gp120 and gp41, two proteins crucial for viral attachment, fusion, and entry into host cells [10, 11]. The viral genome also includes accessory genes, such as tat, rev, nef, vif, vpr, and vpu, in addition to the primary structural genes. These genes encode proteins that regulate transcription, facilitate immune evasion, and enhance viral replication [11, 12].
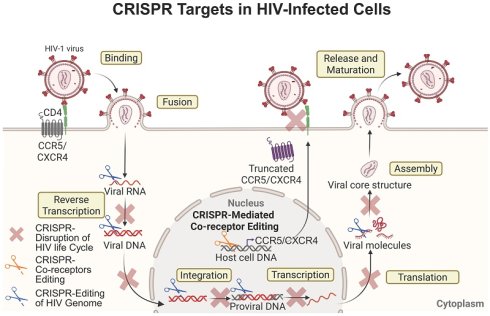
The viral life cycle begins with the binding of the viral glycoprotein gp120 to the primary receptor CD4, followed by attachment to the co-receptors C-C chemokine receptor 5 (CCR5) or C-X-C chemokine receptor type 4 (CXCR4), which are found on the surface of host CD4+ T and myeloid cells [13]. After receptor engagement, a conformational change is triggered by the gp120-CD4 complex, which exposes the binding site of the envelope glycoprotein gp41, mediating the insertion of the viral envelope into the host cell plasma membrane [14]. Once inside the cell, the viral proteins are released into the cytoplasm, and reverse transcriptase reverse transcribes the single-stranded (ss) viral RNA into double-stranded (ds) viral DNA [15]. This newly formed viral DNA is transported into the nucleus and integrated into the host genome to form replication-competent proviral DNA [16]. Subsequently, the host's transcription and translation machinery is used to synthesize and express viral proteins. If the infected cell is activated after therapeutic interruption, newly synthesized viral proteins can assemble into viral particles and be released from the cell as immature virions. These viral particles are then cleaved by HIV-1 protease, which processes viral polyproteins, leading to the formation of mature, infectious virions [17, 18]. The biggest obstacle to HIV elimination is the persistence of these latent viral reservoirs. Shortly after infection, HIV integrates its RNA genome into the host DNA, forming proviral DNA primarily within CD4+ T cells. These cells can remain dormant or expand through clonal proliferation for years, allowing the virus to evade the immune surveillance and remain unaffected by antiretroviral therapy (ART) (Figure 1) [19-22]. Additionally, viral reservoirs vary and exist not only in different cell types (mainly CD4+ T and myeloid cells) but also across various tissues in the body, such as the lymph nodes (LNs), gut, bone marrow, and central nervous system (CNS) (Figure 2) [23-25].
Current ART and CRISPR-Cas9 treatment strategies. Tissue and cell reservoirs of HIV-1 infection (top): CXCR4 (X4)- and CCR5 (R5)-tropic HIV-1 strains preferentially infect CD4+ T cells and macrophages, respectively, and can persist in a latent state within the genome of myeloid and T cells. These cellular reservoirs undergo productive replication or remain transcriptionally silent under active immune surveillance and potent antiretroviral therapy (ART). Homeostatic proliferation of latently infected immune cells in the absence of conventional activation signals leads to their clonal expansion. Upon activation, these latent cells can reactivate and produce new virions; both processes contribute to the maintenance of viral persistence in the host. Viral persistence and immune activation (bottom): Chronic immune activation and inflammation occur in both infected and bystander immune cells, which promote progressive destruction of cells and tissues. Although viral replication is effectively suppressed during ART, treatment interruption results in rapid viral reactivation and rebound, which further causes severe immune and tissue damage. CRISPR-Cas9-based therapeutic strategies aim to target and excise integrated proviral DNA from reservoir cells, thereby preventing viral rebound even after ART cessation. Created with BioRender.com.

Gene delivery and HIV-1 reservoir elimination strategies. HIV-1 reservoirs are protected by anatomical and immunological barriers, which hinder the efficient delivery of gene-editing tools. Local delivery obstacles include poor biodistribution, immune clearance, and off-target accumulation. Current delivery system under development aims to: (1) reduce immunogenicity and improve repeat-dosing; (2) enable cell- and tissue-specific targeting; and (3) enhance biodistribution to the CNS and lymphoid tissues. Additionally, multiple gRNA target sites are needed to excise integrated HIV proviral DNA as well as co-receptor genes such as CCR5 or CXCR4. Together, these advancements aim to enhance in vivo editing efficiency and achieve long-term viral remission or a functional cure. Created with BioRender.com.

1.2 Role of HIV-1 Co-receptors in Pathways for Viral Control
The CD4 receptor is a cell-surface protein mainly found on T lymphocytes and myeloid cells that serves as the primary docking site for HIV-1 [13]. Anti-CD4 nanobodies, such as Nb457, have demonstrated strong potency against diverse HIV-1 genotypes with no reported cytotoxic effects [26]. After HIV binds to the CD4 receptor on T cells, it requires a co-receptor, either CCR5 (for R5-tropic viruses) or CXCR4 (for X4-tropic viruses), or both, to enter the cell (Figure 1). These are G protein-coupled receptors (GPCRs) from the chemokine family [27-29]. Affinity for specific co-receptors affects cell tropism, viral entry, replication, and disease progression. In terms of structural organization, they share key common features, including an extracellular N-terminal domain, three extracellular loops (ECL1-3), and three intracellular loops [30].
The cellular expression patterns of these HIV-1 coreceptors overlap. CXCR4 is broadly expressed on most immune cells (T cells, B cells, and monocytes) and stem cells (bone marrow stem and progenitor cells) [31-33]. CCR5 has a more specialized and selective expression in activated T cells, macrophages, dendritic cells, endothelial cells, vascular smooth muscle cells, mesenchymal stromal cells, and brain-resident microglia [34-36]. However, peripheral blood analysis of HIV-1 infected individuals suggests an upregulation of CCR5 and downregulation of CXCR4 on both CD4+ and CD8+ T cells [37]. This observed effect might be due to the immune environment, especially the presence of inflammatory cytokines such as IL-6, IFN-γ, and granulocyte-macrophage colony-stimulating factor (GM-CSF), which can boost CCR5 expression levels, making mature and activated immune cells more susceptible to infection by R5-tropic HIV strains.
Strategies targeting CCR5 and CXCR4 are used for HIV-1 prevention and treatment. These include the design of co-receptor antagonists and gene-based therapies. Technologies such as clustered regularly interspaced short palindromic repeats-associated protein 9 (CRISPR-Cas9) can disrupt CCR5 or CXCR4 genes, rendering cells resistant to HIV by blocking co-receptor binding (Table 1) [38]. For instance, the application of CRISPR-Cas9 can induce premature stop codons at the CCR5 locus to prevent its expression [39]. CCR5 and CXCR4 have immunoregulatory functions that influence host defense and tissue inflammation, which can also affect HIV-1 replication and sustenance of infection [40]. Studies of HIV-1 elite controllers suggest that they may carry a 32-base-pair deletion in the CCR5 gene (CCR5-Δ32), a mutation that reduces the surface expression of the CCR5 receptor (Figure 3) [29, 41].
Both co-receptors undergo developmental regulation through genetic switches, and HIV exploits these natural patterns by adapting to the most available receptors [42, 43]. Understanding the functional dynamics of each HIV-1 co-receptor has enabled the development of effective treatment strategies. For example, maraviroc, which was approved in 2007, is the first CCR5 antagonist that blocks the entry of R5-tropic strains into host cells [44]. Using a similar strategy targeting the CXCR4 co-receptor, nanobodies were generated from llamas immunized with cells expressing intact CXCR4. Using a counterselection approach, nanobodies that effectively inhibit HIV-1 entry and chemotaxis in vitro have been successfully isolated [45]. Using the natural CCR5-Δ32 mutation as a template, current gene therapy approaches have been used for experimental HIV cures, with some people living with HIV (PLWH) achieving long-term viral control after receiving genetically modified immune cells with mutated CCR5 receptor expression [46-49]. Although these strategies have shown promising results, they are limited by challenges such as incomplete editing, co-receptor specificity, and potential off-target effects [50]. Further mechanistic and therapeutic investigations are required to develop strategies that simultaneously target multiple co-receptors.
The mechanisms aimed at eliminating HIV-1 infection have been previously reviewed [16, 51]. Prior studies have largely focused on selectively targeting reservoir cells based on their immunological characteristics. These reports identified vulnerable stages in the viral life cycle that offer therapeutic potential [52]. Therefore, this review emphasizes the persistent challenge of residual viremia despite combinatorial ART and various immunomodulating strategies. We further examined emerging preclinical strategies that utilize CRISPR-based systems to excise latent viral DNA using targeted delivery approaches. In addition, this review examines the factors that influence therapeutic outcomes in strategies such as shock-and-kill, viral co-receptor disruption, and viral excision, both individually and in combination. This review highlights key knowledge gaps and emphasizes the need to bridge preclinical advances with clinical translation. Finally, we outline the potential synergistic benefits of integrating these approaches to overcome existing barriers and advance toward a functional HIV-1 cure.
2. Pathways for HIV elimination
Advancements in ART have transformed HIV infection from a fatal disease into a manageable chronic condition [53, 54]. However, a functional cure for HIV remains out of reach, mainly due to the persistence of latent reservoirs [54, 55]. In addition, HIV employs multiple immune evasion strategies that further complicate its eradication. One of the biggest challenges is that HIV directly targets CD4+ T cells, gradually depleting key components of the immune response [56]. Infected cells downregulate major histocompatibility complex class I (MHC-I) expression, hindering recognition by cytotoxic T lymphocytes [57]. The virus can also reside in immune-privileged sites, such as the brain, LNs, and gut-associated lymphoid tissue (Figure 2) [57]. Over time, immune exhaustion develops, and the high mutation rate of HIV enables it to escape previously effective immune responses [58]. Therefore, lifelong ART is required in PLWH. However, long-term therapy presents challenges related to adherence, toxicity, cost, and the emergence of drug-resistant viral strains [59, 60]. The burden of comorbidities and limited treatment options further underscore the urgent need for curative strategies in PLWH. Two major therapeutic outcomes are generally envisioned: a functional cure and a sterilizing cure. Functional cure or medicine-free remission is defined as the sustained remission of viral replication in the absence of ART, without evidence of viral transmission, whereas a sterilizing cure represents the complete eradication of replication-competent HIV from the body (Figure 2) [61-64]. Whether the goal is sterilization or functional cure, researchers have sought to achieve these outcomes through diverse approaches (Figure 4), including immune-based interventions that enhance host antiviral responses and gene-editing strategies designed to disrupt key viral or host genomic elements required for infection and persistence [65, 66].
CCR5-Δ32 mutation confers resistance to HIV-1 infection. Wild-type CCR5 (top panel): CCR5 is one of two co-receptors required for HIV entry. The HIV envelope protein, gp120, first binds to the CD4 receptor on the surface of susceptible T cells and macrophages. This binding induces a conformational change in gp120, exposing a binding site for CCR5. Subsequent interaction with CCR5 triggers gp41 to unfold and expose its hydrophobic fusion peptide, which inserts into the host membrane. This facilitates fusion of viral and host membranes, allowing viral entry. CCR5-Δ32 mutation (bottom panel): This 32-base-pair deletion leads to a frameshift that produces a non-functional CCR5 protein that is retained in the endoplasmic reticulum, preventing its expression on the cell surface. As a result, R5-tropic HIV strains cannot infect CD4+ T cells and myeloid cells. Individuals with homozygous CCR5-Δ32/Δ32 genotypes exhibit near-complete protection from HIV-1 infection, whereas heterozygous individuals show reduced viral susceptibility. The discovery of the CCR5-Δ32 mutation has inspired gene-editing and therapeutic strategies aimed at blocking or mutating the CCR5 receptor to achieve viral elimination. Created with BioRender.com.

Current HIV elimination strategies. A) The shock-and-kill strategy targets latent viral reservoirs using LRAs to “shock” the dormant virus into reactivation and render the virus detectable. The active virus then becomes vulnerable to attack by immune effector cells, like cytotoxic T cells (CTLs), or other treatments that “kill” infected cells or induce apoptosis. B) Block and lock approaches employ latency-promoting agents (LPAs) to permanently silence or control latency to prevent reactivation and rebound. This method triggers epigenetic changes that “block” viral transcription and “lock” the integrated virus into a dormant state, making reactivation impossible even if treatment is stopped. C) Vaccination strategies aim to stimulate or enhance humoral and/or cell-mediated immune responses to regulate viral replication and ultimately eradicate reservoirs. These strategies involve designing HIV immunogens, with or without adjuvants, that activate dendritic cells (DCs) to stimulate naïve CD8+ T cells to become CTLs, or B cells to develop into plasma cells that produce HIV-specific antibodies (Abs) capable of killing HIV-infected cells. D) Broadly neutralizing antibodies (bNAbs) are a special type of Abs that can neutralize numerous HIV strains. They target conserved regions on the viral surface, such as Env proteins. Unlike naturally induced antibodies, bNAbs are typically engineered and administered passively rather than produced through vaccination. E) Chimeric antigen receptor (CAR) T-cell therapy involves genetic constructs that encode antigen-recognition chains, often derived from HIV-specific Abs, used to modify T cells of PLWH. These HIV-specific CAR T cells recognize and eliminate HIV-infected cells, including viral reservoirs, through cytotoxic mechanisms that induce apoptosis. F) Programmed death-1 (PD-1) modulation strategies use anti-PD-1 antibodies to target exhausted T cells expressing PD-1, aiming to either remove these T cells or restore their impaired effector functions to boost virus-specific immunity. Created with BioRender.com.

2.1 Immune-based therapies for HIV-1 elimination
2.1.1 Shock and kill
Although the “shock and kill” strategy is one of the most widely studied methods aimed at eliminating latent HIV reservoirs to achieve a sterilizing cure, it has limitations. Using latency-reversing agents (LRAs) to “shock” the virus out of its dormant state makes the previously hidden HIV visible to the immune system, which then “kills” the infected cells [67]. Since this approach was first proposed as a potential HIV-1 cure, researchers have identified more than 160 small-molecule compounds as LRAs [68-70]. For example, plasma-derived exosomes from rhesus macaques selectively fuse with TCR-activated T cells and induce HIV reactivation in resting CD4+ T cells; however, immune control remains ineffective. This is evidenced by increased viral transcription, despite the presence of residual virus [71]. Moreover, while exosomal delivery of HIV-1 Tat showed some efficacy in reversing latency in primary CD4+ T cells, such LRAs have had limited success [72]. Therefore, to effectively eliminate HIV, a synergistic combination of the “shock and kill” strategy and additional complementary approaches must be employed. One such approach involves CD3-targeted adenoviral vectors carrying dCas9-VPR CRISPR activators to trigger suicide gene activation, leading to latency reversal and subsequent viral elimination. This method achieved a modest 57.7% reduction in cells producing productive infection, along with only a 2.4-fold increase in cell death [73]. In addition, ex vivo studies have explored the synergistic combination of IL-15 with HODHBt, a small-molecule inhibitor of protein tyrosine phosphatases [74]. Enhanced HIV-specific granzyme B-releasing T-cell responses were observed in PBMCs from HIV-infected individuals receiving ART, suggesting potential roles in latency reversal and immune activation [74]. Additionally, using a synthetic bryostatin 1 analog and PKC modulator, SUW133, followed by two rounds of natural killer cell treatment during ART in a humanized HIV-infection model, can delay viral rebound after ART interruption [75]. Four out of ten dual-treated mice showed no detectable HIV DNA in their tissues. Each approach highlights the potential of combining LRAs with innate immune effectors to improve HIV clearance. Building on this, studies in simian immunodeficiency virus (SIV)-infected ART-suppressed rhesus macaques have shown that combining the latency-reversing agent AZD5582 with SIV-Env-specific RhmAbs more effectively eliminates proviral DNA from lymphoid reservoirs [76]. However, while there were significant reductions in SIV-DNA in lymph node CD4+ T cells, complete viral elimination was not achieved in this study. Ongoing research involves the use of hybrid polylactic-co-glycolic acid nanoparticles to encapsulate LRAs for HIV-1 reactivation in infected CD4+ T cells. Among these, ingenol-3-angelate has shown promise as it can induce sustained CD4+ T cell activation with low toxicity [77]. Nonetheless, several translational efforts have led to clinical evaluation. For example, a phase 2 clinical trial (NCT05129189) conducted in 2024 involved PLWH on long-term ART [78]. This study tested the effectiveness of combining the anti-PD-L1 antibody ASC22 with Chidamide to reverse HIV latency. Significant increases in cell-associated HIV RNA levels were observed; however, the levels of integrated viral DNA remained unchanged. Based on earlier research, the co-administration of broadly neutralizing antibodies (bNAbs) with LRAs was tested to promote HIV-1 clearance. A phase 2a clinical trial analyzed the effect of the antibody 3BNC117 combined with romidepsin, a histone deacetylase inhibitor used for latency reversal [79]. A delayed viral rebound was observed during analytical treatment interruption (ATI); however, the overall difference was not statistically significant. Despite these efforts, none of these approaches have resulted in a functional HIV-1 cure. The major limitation of the “shock” stage is that current LRAs fail to reactivate all latent proviruses, leaving a significant fraction of intact, replication-competent proviruses non-inducible even after multiple or serial administrations [67]. In the “kill” stage, immune responses are often too weak or exhausted in ART-treated PLWH to effectively clear the reactivated cells [80, 81]. Moreover, some LRAs can trigger widespread immune activation or toxicity, reducing their suitability for long-term use [82]. Together, the lack of highly potent and safe LRAs limits the reliability of the shock-and-kill strategy as a curative approach (Figure 4). Although LRAs alone or in combination with ART are insufficient to achieve a functional cure, integrating potent immune boosters during the “kill” stage or employing gene-editing strategies that target both latent proviruses and newly reactivated viruses may offer promising potential for a functional cure in PLWH [64, 83].
2.1.2 Block and lock
The “block and lock” strategy deploys a means to permanently silence the virus rather than reactivating it [84]. Instead of flushing HIV out of latency, this method uses drugs or genetic tools to “block” the virus in a deeply dormant state, preventing reactivation and replication, even in the absence of ART [84, 85]. Exosomes, immune-tolerant and highly penetrant nanoscale carriers, have been utilized to deliver RNA cargo for epigenetic silencing of HIV-1 in infected cells [86]. When combined with conventional ART, this strategy may reduce dependence on strict treatment adherence in PLWH. This functional cure strategy targets the transcriptional and epigenetic regulatory machinery of HIV-1. Notably, two major categories of block-and-lock agents have been developed: those that disrupt key transcriptional regulators (e.g., Tat inhibitors such as didehydro-cortistatin A (dCA)) and those that modulate epigenetic silencing mechanisms at the HIV promoter level (e.g., RNA-induced silencing and lens epithelium-derived growth factor p75 (LEDGF/p75)-IN interaction inhibitors (LEDGINs)) [87-92]. However, the challenge lies in the complete and consistent silencing of all proviral DNA across various tissues and reservoir sites. Many current compounds do not fully penetrate all cellular reservoirs or maintain the long-term suppression of viral replication necessary for complete silencing; thus, the block-and-lock strategy does not permanently silence HIV [93].
2.1.3 Therapeutic vaccines
Therapeutic vaccines have been developed to stimulate the immune system in PLWH, aiming to improve their ability to recognize, control, or even eliminate the virus in combination with ART [94]. Unlike preventive vaccines, these vaccines are designed to strengthen the body's natural defenses, suppress viral levels, and achieve viral clearance [94]. A major challenge is that HIV rapidly mutates and evades the immune system of the host. Additionally, immune exhaustion caused by chronic HIV infection reduces vaccine efficacy [95, 96]. Latent reservoirs are also unaffected by these immune responses, allowing the virus to persist [23]. Recently, first-in-human studies of the HIVconsvX T-cell vaccine demonstrated its safety and broad immunogenicity in HIV-negative adult patients. In this phase 1 trial, all participants produced strong T-cell responses that recognized multiple conserved HIV-1 epitopes across the major global clades. Vaccine-induced T cells showed functional versatility, proliferated upon antigen re-exposure, and inhibited HIV-1 in vitro, supporting the potential of T-cell-focused immunogens as a therapeutic strategy to target HIV reservoirs and improve viral control [97]. To date, therapeutic vaccines have not resulted in durable viral control [98].
2.1.4 Broadly neutralizing antibodies
Broadly neutralizing antibodies (bNAbs) are designed to target the hard-to-reach regions of the HIV envelope, allowing the neutralization of several viral strains [99]. They have been used in both preventive [100-102] and therapeutic settings [103, 104], often alongside ART to reduce viral load and delay viral rebound. Preclinical studies have demonstrated that combining bNAbs with ART or LRAs significantly delays viral rebound in humanized mice [105] and macaques [106]. Notably, in simian-human immunodeficiency virus-infected ART-suppressed macaques, dual therapy with the IL-15 super-agonist N-803 and bNAbs triggered transient viremia that reprogrammed CD8+ T cells, achieving sustainable viral remission in approximately 70% of animals, despite only modest reductions in the viral reservoir [107]. These findings underscore that enhanced immune responses, rather than complete reservoir eradication, can sustain post-ART viral control, highlighting the translational potential of immune-based HIV remission strategies in clinical practice. Recent clinical trials have provided additional evidence that bNAbs can delay viral rebound and allow partial virologic control without ART in humans. In the phase 2a TITAN trial, the administration of bNAbs (3BNC117 and 10-1074) delayed viral rebound upon ART interruption, with 36% of participants maintaining partial or complete control over 25 weeks despite subtherapeutic antibody levels [108]. The antibody-mediated prevention study further demonstrated that among Southern African women who received VRC01 or placebo near HIV acquisition, 18% maintained ART-free viral suppression for ≥32 weeks, with one VRC01 recipient maintaining viral loads below 200 copies/ml for nearly two years [109]. These findings imply that the early administration of bNAbs, especially alongside ART, may improve post-treatment viral control in patients with HIV. Recently, a phase 1/2a trial of a triple-bNAb combination (PGT121, PGDM1400, VRC07-523LS) in PLWH demonstrated that 83% of participants sustained virologic suppression for at least 28 weeks, with 42% achieving prolonged control for 38-44 weeks, even after antibody levels decreased [110]. This long-term control is associated with reduced immune activation, T cell exhaustion, and proinflammatory signaling [110]. These results suggest that triple-bNAb therapy may offer more durable ART-free viral suppression than dual-bNAb therapies. However, the effectiveness of bNAbs is limited by several factors, as HIV can mutate and evade even the most broadly acting antibodies, leading to resistant strains and subsequent rapid viral escape [99, 111]. Moreover, not all PLWH respond favorably to bNAbs, and the antibodies typically require repeated administration to maintain their effect, further rendering them ineffective as a cure for HIV [99].
2.1.5 Chimeric antigen receptor (CAR) T-cell therapies
Chimeric antigen receptor (CAR) T-cell therapy, originally developed for cancer treatment, has been adapted as a potential strategy for curing HIV by engineering T cells to recognize and kill HIV-infected cells [112]. These modified T cells target HIV-1-specific antigens or conserved parts of the virus, such as envelope proteins, in the infected cells [113]. Anti-HIV-1-engineered CAR T-cells have shown promising results, demonstrating high specificity for infected T-cells, suppression of viral replication, and delayed viral rebound [114-116]. However, CAR T-cells are unable to fully reach viral reservoirs in deeper tissues [117-120]. The only successful CAR T-cell model was developed in macaques treated with hematopoietic stem cell (HSC)-derived CAR T-cells [117, 120]. These cells proliferate within lymphoid germinal centers and are detectable in specific brain regions, including the hippocampus and parietal cortex, in most macaques. Nevertheless, their trafficking to other parts of the CNS, such as the basal ganglia, thalamus, and cerebellum, is limited and inconsistent [117, 120, 121]. A major challenge is that HIV rapidly mutates and can downregulate or hide target antigens, such as env epitopes, making it harder for CAR T-cells to recognize the infected cells [117, 120, 122, 123]. Additionally, persistent inflammation and T-cell exhaustion in chronic HIV infection can impair the longevity and effectiveness of CAR-T cell responses in patients with HIV. Finally, CAR T-cells may struggle to penetrate and function within sites such as the LNs and the brain, where latent HIV often resides [84, 124]. However, CAR T-cell therapy has not yet achieved durable viral remission in PLWH.
2.1.6 Immune checkpoint modulation
Immune checkpoint modulation offers another approach, aiming to enhance the immune system's ability to fight HIV by blocking proteins, such as programmed cell death protein 1 (PD-1) and cytotoxic T-lymphocyte-associated protein 4 (CTLA-4), which normally act as “brakes” on T-cell activity [125]. The goal of inhibiting these checkpoints is to revive exhausted HIV-specific T cells, helping them to better recognize and eliminate HIV-infected cells. Although this strategy has shown promise in cancer immunotherapy, its application in HIV treatment presents several challenges. In HIV, immune checkpoint blockers only produce modest improvements in T cell function and viral control, and they also risk excessive immune activation and inflammation [95, 126, 127]. Moreover, reversing T cell exhaustion may not significantly increase viral clearance from latent reservoirs, limiting progress toward an HIV-1 cure [128].
2.1.7 Immune challenges for HIV-1 elimination
Despite advances in ART and other therapies, the complexity of the virus, including immune evasion, latent persistence, and rapid mutation, continues to hinder the development of a definitive cure [129]. However, approaches such as LRAs, gene editing, and therapeutic vaccines show promise, although each faces unique obstacles that limit their effectiveness [129, 130]. A notable example is CAR T-cell therapy, which has faced several challenges. These include HIV's ability to infect and destroy CAR T-cells themselves, difficulty in targeting hidden viral reservoirs, high mutation rates, viral escape, and cytokine release syndrome (CRS), which can cause mild, flu-like symptoms or life-threatening multi-organ failure, all linked to CAR T-cell activity. Additionally, the low expression of viral antigens on infected cells and the high manufacturing and logistical costs of CAR T-cell therapy present significant limitations [131, 132]. Importantly, CAR T-cells alone have not yet prevented viral rebound after ART interruption [133]. Recent advances in gene editing have opened new possibilities. Studies have shown that CRISPR-Cas9-mediated integration of anti-HIV CARs into the CCR5 locus creates HIV-resistant T cells, preventing the infection of CD4+ CARs and preserving their cytotoxic function. Using single-chain variable fragments from bNAb 10-1074, these CAR T-cells specifically eliminated HIV-infected cells in vitro and temporarily limited infection in peripheral blood mononuclear cell-derived humanized mice [134]. This approach also demonstrated functional expansion in vivo, highlighting the potential of CCR5-disrupted CAR T cells to improve therapeutic outcomes. Continued research, new combination therapies, and further extended development of CAR T-cells are essential to overcome these barriers and move toward a functional HIV cure.
2.2 Gene editing therapies
Gene editing has become a transformative tool in modern biology, enabling the precise manipulation of genetic material in living organisms [135]. These strategies leverage the body's natural DNA repair pathways to introduce targeted insertions, deletions, or sequence replacements into the host's genome. Early methods, such as zinc-finger nucleases (ZFNs) and transcription activator-like effector nucleases (TALENs), proved the feasibility of engineered nucleases for site-specific genome modification; however, they are limited by complex protein design and low scalability [136]. The emergence of the CRISPR-Cas system, adapted from a bacterial immune mechanism, has revolutionized genome engineering by providing an easily programmable, cost-effective, and versatile platform with broad applications across model organisms and in clinical settings [137]. Recent studies have developed a modified CRISPR enzyme, CasX2Max, which carries three amino acid substitutions that enhance the sgRNA-DNA binding and catalytic efficiency in HEK293-FT cells. These modifications make CasX2Max a promising tool for precise CCR5 gene disruption [138].
2.2.1 ZFNs and TALENs
ZFNs and TALENs are considered first-generation gene-editing tools [136]. ZFNs are chimeric nucleases created by combining a zinc-finger DNA-binding domain with the nuclease domain of an FokI-type type IIS restriction endonuclease [139]. Each ZFN binds specifically to a set of three base pairs and can be combined to recognize longer DNA sequences, thereby enhancing the specificity and effectiveness of gene targeting [140]. Another essential part of ZFNs is the restriction endonuclease domain, which facilitates DNA cleavage [140]. This feature enables ZFNs to be re-engineered to target specific sites within the human genome [141]. Several studies have shown that ZFN-mediated disruption of the CXCR4 gene in CD4+ T cells confers resistance to HIV [142, 143]. Compared to lentivirus-delivered CXCR4-targeting short hairpin RNAs, ZFN-modified cells displayed sustained enrichment and reduced HIV-1 viral loads in vitro and in vivo, indicating that CXCR4 modification is a promising genetic approach for HIV resistance [143]. ZFNs have also been used to simultaneously disrupt CCR5 and CXCR4 genes in primary human CD4+ T cells, resulting in normal proliferation and strong resistance to both CCR5- and CXCR4-tropic HIV-1 strains in vitro [142]. However, in a humanized mouse model, these gene-modified cells were successfully engrafted and trafficked normally, but resistance to HIV-1 infection was only temporarily observed in vivo [142].
TALENs are another class of naturally derived gene-editing tools similar to ZFNs that have demonstrated efficacy in editing host genes, such as CCR5 and CXCR4, the proviral integration-associated protein LEDGF/p75, and long terminal repeat (LTR) regions of HIV proviral DNA [144, 145]. Preclinical studies have provided proof-of-concept that TALEN proteins can be effectively encapsulated within a nanocapsule-based delivery system for efficient gene editing (ex vivo) in primary HIV-1 reservoir cells, such as T cells and macrophages [146]. The authors adopted an in situ polymerization technique to wrap TALEN proteins encapsulated in cationic polymeric shells, specifically targeting the HIV-1 transcription activator-responsive region [146]. The effectiveness of HIV-1 gene editing using this nanocapsule was further confirmed by the observed reduction in HIV-1 p24 expression in latently infected T cells [146]. However, the inherent complexity and large size of TALENs, along with difficulties related to their efficient packaging, delivery, and scalability, continue to pose significant challenges for successful clinical translation [136, 144, 145].
Although these early preclinical tests demonstrated the possibility of modifying CXCR4 and/or CCR5 to prevent or treat HIV infections, the labor-intensive nature of protein engineering and limited scalability have restricted their broad application [144]. These obstacles have been addressed through the development and adoption of CRISPR-Cas systems, which are natural bacterial defense mechanisms that have become transformative genome-editing tools owing to their simplicity, versatility, and high specificity [135, 147]. CRISPR technologies have shown promise in preclinical animal models by targeting either the HIV genome or essential co-receptors, such as CCR5 and CXCR4 [38, 148]. Advances in materials science and chemical engineering have facilitated the development of versatile and more effective delivery platforms, offering improved precision and safety for CRISPR-based therapies compared with earlier generation tools [149, 150].
2.2.2 CRISPR-based HIV-1 cure strategies
Early CRISPR efforts primarily targeted the viral genome, often LTRs or essential genes, to excise or inactivate the provirus [151-154]. However, incomplete editing, rapid viral escape, and delivery constraints limit the durability of viral inactivation [155]. Consequently, the focus has shifted to genetically stable host entry factors, especially CCR5 and CXCR4, and combination treatments that combine co-receptor editing with ART and/or proviral removal [156]. Although initial studies targeted the provirus directly [143, 157], new evidence indicates that long-term HIV control requires both the prevention of new infections and the depletion of viral reservoirs [158]. This has led to a strategic shift toward co-receptor editing and multimodal therapeutic approaches. Building on these findings, current research more often combines CRISPR disruption of CCR5 and CXCR4 with long-acting ART or proviral removal to block viral spread and progressively diminish latent reservoirs (Figures 4 and 5; Table 1) [159, 160]. Screening for CRISPR editing success is typically performed on CD4+ T cells and HSCs. One of the earliest studies demonstrated the superior efficiency of CCR5 editing compared with previous methods [161]. Using lentiviral vectors that express Cas9 and single-guide RNAs (sgRNAs) targeting CCR5, a single transduction into HIV-1-susceptible human CD4+ cells resulted in significant CCR5 gene disruption, with approximately 43% of the cells exhibiting CCR5 disruption. These CCR5-disrupted cells were resistant to R5-tropic HIV-1 and had a selective advantage over unmodified cells during infection [161]. Additionally, a T7 endonuclease I assay used to check for off-target mutations in stably transduced cells found no off-target effects. Similarly, researchers have explored whether adenovirus-delivered CRISPR-Cas9 can effectively edit CCR5 in primary human CD4+ T cells [162]. They isolated cells from donors, delivered the CRISPR-Cas9 system via adenoviral vectors, and tested the susceptibility of the cells to HIV infection. They successfully disrupted CCR5 in 74.1 and 63.8% of primary T cells from the two donors, respectively. These edited cells also showed resistance to CCR5-tropic HIV-1, with resistance levels similar to those reported in previous studies (Table 1) [162]. To further examine CCR5 as a therapeutic target, Wang et al. studied whether targeting CCR5 in human induced pluripotent stem cells (iPSCs) using CRISPR could create immune cells resistant to CCR5-tropic HIV-1 [163]. Editing frequencies reached 27% with single guide RNAs and 41% with dual guide RNAs for biallelic disruption, respectively. These results indicate that homozygous CCR5 mutations confer resistance to CCR5-tropic HIV-1, suggesting that iPSC-derived CCR5-disrupted cells could be a source of HIV-resistant immune cells. To further investigate the role of HIV-1 co-receptors, CCR5 and CXCR4 genes were simultaneously disrupted in human CD4+ T cell lines using CRISPR-Cas9, achieving editing efficiencies of 55 and 36%, respectively [164]. The edited cells showed resistance to both HIV-1NL4-3 (CXCR4-tropic) and HIV-1YU-2 (CCR5-tropic) strains [164]. Moreover, studies have indicated no significant difference in apoptosis between gene-edited and unmodified cells based on flow cytometry with 7-AAD and annexin V, which assess cellular death and apoptosis, respectively [165]. Deep sequencing and T7E1 assays of the predicted off-target sites revealed no detectable off-target effects. A recent study focused on disrupting CXCR4 and CCR5 by introducing stop codons using base editing in primary human CD4+ T cells [39]. Flow cytometry showed that CXCR4 expression decreased by 75 and 86% on day 4, whereas each guide RNA achieved an 80-94% reduction in CCR5 expression by day 11. To evaluate T cell function, cytokine production (IL-2, IL-4, IFN-γ, and TNF-α) was measured in both control and dual-receptor-edited T cells, which showed similar levels of cytokine production, indicating that these cells retained their functional abilities. Finally, the ability of co-receptor knockout cells to resist HIV infection was tested using replication-incompetent lentivirus pseudotypes with CCR5- or CXCR4-tropic HIV-1 envelopes. The edited cells exhibited a significant reduction in co-receptor expression and viral infection [39].
Strategic HIV elimination targeting cellular and tissue reservoirs using CRISPR-Cas9. CRISPR-Cas9-based systems provide high specificity for latent proviral DNA and represent a promising approach for eliminating viral reservoirs. In this system, viral guide RNAs (gRNAs) recognize complementary sequences in latent HIV DNA, which are then excised by Cas enzymes. Beyond targeting viral DNA, CRISPR-Cas9 can also be used to disrupt host genes (for example, CCR5 or CXCR4) to block co-receptor binding, inhibit viral entry, and suppress replication. CRISPR-Cas9 technology can intervene at multiple stages of the HIV life cycle, including reverse transcription, integration, viral protein transcription, and assembly, thereby disrupting viral core formation and replication. Despite its genetic specificity, delivery to infected cells remains a major challenge. Viral vectors (e.g., adeno-associated viruses (AAVs)) or LNPs are commonly used; however, optimizing efficient delivery to all reservoir cells is ongoing. To better target immune cells within viral reservoirs, strategies to incorporate ligands for immune cell receptors, such as for CCR5 and/or CXCR4, into the delivery platforms are anticipated to improve target specificity and delivery efficiency. Preclinical testing of targeted CRISPR-Cas9 delivery systems is currently undergoing in laboratory settings, including HIV-infected CD4+ T cells and macrophages, small rodent models, and SHIV-infected macaques, with eventual translation to HIV-1-infected subjects. While the delivery and excision specificities of CRISPR-Cas9 systems are promising, potential limitations that may affect treatment outcomes include off-target editing of the host genome, inefficient delivery to latent reservoirs, endosomal degradation of LNP cargo, immunogenicity to bacterial CRISPR-Cas9 components, emergence of HIV escape variants, and possible toxicities. Created with BioRender.com.

CXCR4 and CCR5 receptor gene editing and HIV-1 elimination
| Year | CRISPR Modifications | Duration or Dose | Outcomes | Ref. |
|---|---|---|---|---|
| 2015 | Adenovirus delivery of CRISPR-Cas9 with sgRNAs to disrupt CCR5 in primary CD4+ T cells and conferring HIV-1 resistance. | CCR5 gene editing in primary CD4+ T cells was achieved using the Ad5F35 adenoviral vector at a MOI of 30 or 100, with maximal editing at 8 days. | Up to 74% indels, effectively eliminating CCR5 in primary CD4⁺ T cells. This confers resistance to HIV-1 infection. | [162] |
| 2015 | CRISPR/Cas9-mediated disruption (knockout) of the CXCR4 gene in human primary CD4⁺ T cells to block HIV-1 entry and create HIV-resistant immune cells. | IL-2 treated primary human CD4⁺ T cells were stimulated with anti-CD3/CD28 for 2-3 days, electroporated with 2 μg CXCR4-gRNA-Cas9 plasmid/5×106 cells, cultured for 2 days, then assessed after 6 to 8 hours HIV-1 exposure. | CRISPR/Cas9 disruption of CXCR4 in primary human CD4+ T cells reduced HIV-1 infection by >64% at day 7 compared to control cells. | [159] |
| 2017 | Targeted knock out of CCR5 gene in human CD34+ hematopoietic stem/progenitor cells. | Analysis of human hematopoietic reconstitution and CCR5 disruption in mice from 6 to 12 weeks post-transplantation, with key evaluations performed at week 12. | CCR5-disrupted mice maintained 94% of their CD4+ T cells compared to 37% in controls. | [169] |
| 2019 | CRISPR-edited CCR5-ablated HSPCs and progenitor cells were transplanted into an HIV-1 infected patient. | The patient received a single infusion of CRISPR-edited CD34+ along with unedited cells after myeloablative (cyclophosphamide and total-body irradiation) conditioning. Follow-up included 4-weeks of ART interruption at 7 months. | CRISPR-mediated CCR5 disruption ranged from 5 to 8% in bone marrow cells over 19 months post-transplant, demonstrating long-term engraftment of edited HSPCs but with insufficient efficiency to cure HIV-1 infection. | [194] |
| 2021 | Disrupt the CCR5 gene in HSCs to create HIV-resistant immune cells. | Refers to generally low-dose CCR5-edited HSPC infusion. | Disrupting the CCR5 gene in HSCs aims to create HIV-resistant immune cells, inspired by the 0% increased mortality in CCR5-∆32 homozygotes and the 31.2% efficacy seen in the RV144 HIV vaccine trial. | [169, 189, 190] |
| 2022 | Disruption of CCR5 and CXCR4 genes in T cells and HSPCs, creating resistance to multiple HIV-1 strains. | Cas9/gRNA was given to human CD4+ T cells by electroporation, analyzed gene editing, and results assessed in mice up to six weeks. | CRISPR-Cas9 disruption achieved up to 88% reduction of CCR5 and CXCR4 in primary T cells, with editing efficiencies of 22-62% in HSPC and T cells. There was resistance to multiple HIV-1 strains. | [38] |
| 2023 | Targeted CCR5 gene and HIV-1 proviral DNA. | ART was for 4 weeks, followed by a recovery period, then CRISPR therapy. | Elimination of HIV -1 proviral DNA in lymphoid, bone marrow, and CNS tissues in 58% of infected animals. | [148] |
| 2025 | Knocked out CCR5 gene in human stem cells. | Mice were transplanted with 106 HSPCs in five doses of CCR5 edited HSPCs. The balance of HSPCs comprising mock edited (GFP gRNA) cells. | The results showed over 90% protection against HIV infection. | [170] |
| 2025 | To remove latent HIV-1 proviral DNA from infected CD4+ T cells. | Repeated dosing of targeted LNPs carrying CRISPR. | Repeated LNP dosing in ART-treated humanized mice achieves 80% HIV-1 DNA excision. | [184] |
Building on the success of early studies, CRISPR-based strategies have been developed for animal studies [38, 166-168]. A single CRISPR-Cas9 editing system was used to disrupt CCR5 in human CD34+ HSCs (Table 1) [169]. The edited HSCs were transplanted into humanized NOD.Cg-Prkdcscidll2rgtm1Wjl/SzJ (NSG) mice, which were subsequently challenged with HIV-1. Efficient and durable CCR5 excision in T cells from long-term HSCs was observed, and mice that received edited cells exhibited significantly reduced HIV-1 RNA levels. This study demonstrated that CRISPR-Cas9-mediated CCR5 disruption in long-term repopulating HSCs is both feasible and effective, supporting the potential of CCR5-edited HSCs as a therapeutic strategy for HIV-1 [169]. A similar study was conducted targeting the CXCR4 receptor using CRISPR-Cas9 in primary human CD4+ T cells [159], in which four gRNAs that efficiently induced indel mutations in the CXCR4 gene were identified. Following lentiviral transduction with CXCR4-targeting gRNAs, the proportion of CXCR4-expressing cells decreased by 70-77%. To assess the protective effect of CXCR4 disruption, the cells were challenged with a CXCR4-tropic HIV-1 strain. In CXCR4-edited cells, viral expression was completely absent, whereas 55% of the infected control cells showed detectable viral activity [159]. Another study identified four gRNAs that efficiently induced high-frequency editing of the human CCR5 gene [170]. When introduced into primary T cells, all four gRNAs successfully disrupted CCR5, leading to a significant reduction in the proportion of CD4+ and CD8+ T cells expressing surface CCR5. To assess the impact on HIV susceptibility, stimulated human PBMCs were electroporated with Cas9 and either CCR5-specific gRNAs or a control GFP-specific gRNA and then challenged with a high dose of CCR5-tropic HIV‑1JR-CSF. CCR5-edited CD4+ T cells showed a sustained reduction in HIV infection compared to those treated with GFP gRNA. Importantly, the degree of infection resistance correlates with a decrease in CCR5+ CD4+ T-cells, supporting CCR5 editing as an effective strategy to confer resistance to HIV in human T-cells [170]. A preclinical study was conducted to confer HIV resistance by simultaneously disrupting CCR5 and CXCR4 [38]. Successfully edited T lymphocytes reduce the surface expression of both co-receptors, resulting in resistance to R5, X4, and dual-tropic HIV-1 strains. In addition, disrupted CCR5 alleles in human CD34+ hematopoietic stem and progenitor cells (HSPCs) generate HIV-resistant macrophages. In humanized mice, HSPCs with dual co-receptor disruption showed poor engraftment in the bone marrow and reconstitution of CD4+ T cells, whereas CXCR4-disrupted CD4+ T cells were enriched in the peripheral blood and spleen after the HIV-1 challenge. These results likely reflect the survival advantage conferred by resistance to viral infections [38].
2.2.3 Immune and Safety Implications for CCR5 and CXCR4 Disruption
Although modifying both CXCR4 and CCR5 receptors is promising for conferring broad resistance to HIV-1, it raises important concerns because of their fundamental roles in immune system regulation. CXCR4 is critical for HSC homing, retention, and migration within the bone marrow niche and plays a key role in thymic T cell development and lymphoid tissue organization [171]. Therefore, disruption of CXCR4 function may impair hematopoiesis, reduce thymic output, and disturb the normal immune cell distribution. CCR5, on the other hand, is essential for the recruitment and activation of immune cells, such as T cells and macrophages, during inflammatory and infectious responses [172]. Loss of this receptor may lead to altered immune surveillance, diminished responsiveness to pathogens, and dysregulated cytokine signaling. Consequently, the simultaneous disruption of both CXCR4 and CCR5 can compromise immune homeostasis and weaken host defenses against infection or vaccination. Therefore, long-term risk management is essential, as such interventions may increase susceptibility to opportunistic infections, cause immune dysregulation, impair CAR-T cell trafficking to target sites, and lead to other immune-related complications. Although short-term in vitro studies have demonstrated that dual-edited cells remain viable and functionally competent, the long-term immunological consequences remain insufficiently characterized and require comprehensive evaluation before clinical application [165]. The CXCR4/CXCL12 and CCR5/CCL5 signaling axes are key mediators of crosstalk between malignant cells and the tumor microenvironment, playing critical roles in the migration and metastasis of epithelial malignancies [173]. Building on this understanding, preclinical studies have demonstrated the therapeutic efficacy of CXCR4 and CCR5 antagonists in limiting tumor progression [174, 175]. Although the long-term oncological effects of HIV-1 co-receptor editing remain largely unexplored, the therapeutic repositioning of HIV drugs targeting these receptors is being investigated in oncology. This approach is based on the rationale that disrupting CXCR4 and CCR5 functions can suppress the migratory and metastatic potential of malignant tumors, offering a promising avenue for anticancer therapy [176].
3. Combinatorial therapies for viral elimination
Combinatorial approaches that simultaneously target viral co-receptors and other critical stages of the HIV life cycle and replication have gained increasing attention because of their improved therapeutic efficacy compared with monotherapies [177-179]. Recent CRISPR-Cas9-based gene therapies, such as CCR5 gene editing and proviral excision, have shown considerable promise but have also highlighted persistent challenges related to in vivo delivery, editing efficiency, and the long-term persistence of edited cells [178].
Recent studies have explored multimodal strategies to overcome these limitations. In this context, Herskovitz et al. reviewed the application of CRISPR-Cas9 to eliminate latent HIV-1, highlighting its potential and addressing critical challenges related to delivery, precision, and safety [180]. Building on this, they demonstrated that CRISPR-Cas9 mRNA combined with TatDE gRNAs and delivered with lipid nanoparticles (LNPs) efficiently and specifically disrupts multiple HIV-1 exons, enabling the excision of latent proviral DNA across diverse viral strains and underscoring a promising gene-editing strategy for HIV-1 eradication [181]. A recent study treated HIV-1-infected humanized NSG mice with a combination of long-acting ester ART prodrugs and CRISPR-Cas9-mediated gene-editing constructs targeting both CCR5 and HIV-1 proviral DNA sequences [148]. CCR5 gene editing targets specific regions, including CCR5Δ32 deletion, which yields cells lacking CCR5 expression and are resistant to infection by CCR5-tropic HIV-1 [148]. Following viral infection, the mice underwent a three-step treatment protocol that included a long-acting, slow-effective release ART (LASER-ART) regimen comprising nanoformulated myristoylated cabotegravir, lamivudine, abacavir, and native rilpivirine. This regimen suppressed viral replication in conjunction with CCR5 gene editing using CRISPR-Cas9. The subsequent step involved the use of AAV9-CRISPR-Cas9 to remove the targeted proviral DNA sequences, specifically by cleaving the LTR-Gag region. Notably, 58% of the animals in the ART and dual CRISPR treatment groups displayed undetectable plasma viral RNA levels. Results from reservoir tissues indicated that the combinatorial strategy, including LASER-ART, CCR5 gene editing, and HIV-1 CRISPR, was more effective than separate treatments in reducing viral DNA levels [148].
Similarly, a dual gene-editing approach was developed to create cells resistant to both CCR5-tropic and CXCR4-tropic HIV-1 strains [182]. This method involved using CRISPR-Cas9 to knockout CCR5 while expressing C46, a membrane-bound HIV-1 fusion inhibitor, in the cells. In a human T-cell line model, cells showed significantly reduced HIV-1 replication and increased survival after exposure to CCR5-tropic or CXCR4-tropic HIV-1 strains [182]. Additionally, rilpivirine-loaded LNPs functionalized with a CCR5 ligand successfully targeted myeloid cell reservoirs and crossed the blood-brain barrier, highlighting the potential of CCR5-targeted delivery systems for CRISPR-Cas9-based HIV therapy [183]. Recently, our group has developed CXCR4 ligand-functionalized LNPs designed for the targeted delivery of CRISPR-Cas9 and gRNAs to eliminate latent HIV-1 from CXCR4-expressing cells [184]. These LNPs improved mRNA translation and cellular uptake through CXCR4-mediated mechanisms, enabling the efficient removal of HIV-1 DNA from infected CD4+ T cells. We used two lymphocytic cell lines with high CXCR4 expression to demonstrate the cell-specific mRNA delivery. Recognizing the challenges of transfecting CD4+ T cells, this study focused on creating cell-selective CXCR4-targeted LNPs (T-LNPs) to ensure the effective delivery of CRISPR-m1Ψ-mCas9-gRNA for LNP uptake and subsequent HIV-1 DNA excision within T cells. The use of targeted LNPs resulted in an 80% overall excision of HIV-1 DNA in lymphocytes after multiple doses. In humanized mouse models, the combination of ART with receptor-targeted LNPs resulted in approximately 60% excision efficiency in the blood and spleen tissues. This underscores the potential of targeted LNPs to specifically target and reduce HIV-1 proviral DNA in latently infected and ART-suppressed lymphoblasts (Figure 5) [184]. Notably, to explore CXCR4 as a therapeutic target for HIV, a naturally occurring human CXCR4 mutant, P191A, was generated using a combination of CRISPR and PiggyBac transposon technologies [185]. Treatment with either two distinct gRNAs or a duplex CRISPR system resulted in a significant reduction in the CXCR4+ targeted cell population from 99.8 to 18.4%, 12.0%, and 11.6%, respectively. DNA sequencing confirmed a homozygous P191A mutation. When these cells were infected with HIV-1NL4-3, a 50% decrease in HIV-1 replication was observed compared to that in wild-type cells, indicating that the P191A mutation confers resistance to HIV-1. Although these approaches demonstrate strong viral suppression and elimination of latent proviral DNA, their greatest potential may lie in thoughtfully designed combinations that incorporate newly developed ultra-long-acting ART (ULA-ART), latency reversal, immune clearance, and gene editing. For example, the “shock-and-kill” strategy reactivates latent viruses using LRAs, allowing for immune clearance or targeted gene editing. When combined with CRISPR, this could increase Cas9 access to reactivated proviruses, thereby boosting editing efficiency.
Conversely, in a “block-and-lock” model aimed at deepening latency, CRISPR could be redundant unless it is used for permanent silencing or excision of the target gene. Another promising approach is the combination of bNAbs and CRISPR systems. bNAbs may help eliminate reactivated infected cells or prevent reinfection after CRISPR-based proviral DNA excision, potentially serving both therapeutic and prophylactic roles. However, the timing, immune engagement, and potential immunogenicity of CRISPR components must be carefully optimized to avoid redundancy or adverse effects. Table 2 compares the different HIV cure strategies used. It focuses on combinations such as CRISPR with ART, immunotherapy, LRAs, bNAbs, and engineered T cells. The table shows how these strategies work together. It also lists their benefits, drawbacks, research progress, and potential risks. Overall, although no single combination has yet achieved consistent HIV eradication, available evidence indicates that the combination of CRISPR with pharmacological and immunological approaches provides synergistic benefits in HIV treatment. Future improvements should focus on enhancing delivery methods, reducing immunogenicity, and customizing the regimen timing to maximize synergy and prevent redundancy. Such thoughtfully designed combinations are the most promising path toward sterilizing or functional HIV-1 cures.
4. Lab-to-clinic pathways to achieve an HIV cure
Although CCR5 gene editing has shown significant promise in in vitro studies and animal models, its clinical application in PLWH has been limited to a few isolated cases and has not yet been broadly adopted [186]. Several clinical trials have been conducted based on various HIV-1 cure strategies that primarily aim to achieve substantial viral suppression with ART while targeting different aspects of HIV-1 pathogenesis.
Combinatorial HIV-1 Cure Strategies
| Strategy | Key Components | Synergy / Advantages | Risks / Limitations | Status | Ref. |
|---|---|---|---|---|---|
| Shock-and-Kill + CRISPR | CRISPRa or LRAs + CRISPR editing | Latency reversal increases proviral accessibility for CRISPR excision | Limited in vivo validation; risk of incomplete editing and off-target effects | Preclinical (cell models, proof-of-concept) | [83] |
| LASER-ART + CRISPR | Long-acting ART + AAV9-CRISPR targeting LTR/Gag | Dual suppression + proviral excision; reduced rebound; tissue clearance | Partial cures in mice; delivery efficiency and off-target risk | Preclinical (humanized mice) | [158] |
| CRISPR + ART (EBT-101) | AAV9-SaCas9 + gRNAs with suppressive ART | Multiplex targeting lowers viral escape: ART maintains suppression during editing | Viral rebound in early trial; incomplete eradication of latent reservoirs | Phase I/IIa (first-in-human) | [196, 197] |
| Immunotherapy + LRAs | AGS-004 dendritic vaccine + vorinostat | Safe; modest T-cell induction; partial reservoir effects | No persistent impact on replication-competent reservoir | Early clinical trial | [198] |
| Shock-and-Kill + bNAbs | Vorinostat + long acting bNAbs | Potential immune clearance of reactivated cells | Weak LRA potency; limited reservoir reduction | Phase I trial | [226] |
| bNAbs + Immune Modulators | bNAbs + IL-15 superagonist or TLR7 agonist | Enhances immune clearance; delayed viral rebound in macaques | Anti-drug antibody responses; incomplete reservoir elimination | Preclinical (SHIV models) | [107] |
| CRISPR-Engineered CAR T Cells | CRISPR/Cas9-mediated CCR5 disruption + CAR integration (10-1074 bNAb scFv) | CCR5 knockout confers resistance; CAR T-cells eliminate HIV-infected cells; in vivo expansion | Limited to R5-tropic strains; partial editing; viral escape; transient suppression | Preclinical (in vitro, hu-PBMC mice) | [134] |
| CRISPR Dual Targeting | CCR5 knockout + C46 fusion inhibitor | Broad protection against R5 and X4 HIV-1 strains | Tested only in cell lines; vector immunogenicity | Preclinical | [182] |
| CXCR4-Targeted LNPs + CRISPR | CXCR4 receptor and lymphoid tissue targeted LNPs + CRISPR + ART | Selective T-cell targeting; approximately 60 to 80% proviral excision | Delivery scalability; tissue variability | Preclinical (in vitro, hu mice) | [184] |
| Block-and-Lock (CRISPR/dCas9-KRAB) | dCas9 repressors targeting HIV LTRs | Persistent latency; prevents reactivation | Requires sustained expression; safety unknown | Preclinical | [227] |
| CRISPR-Edited HSPCs | CCR5-edited stem cells + ART | Long-term engraftment; partial immune protection | Rebound after ART interruption | First-in-human (case study) | [194] |
These approaches mainly include the eradication of multiple viral reservoirs across anatomical and cellular compartments, attaining strong control of viral replication through immune-enhancing, and combination therapies that synergistically integrate with immune-boosting and reservoir-eliminating modalities [187]. One of the first trials to assess CCR5 gene editing in humans employed ZFN-mediated modification of autologous CD4+ T cells (NCT03666871) [188]. In a non-randomized study involving 12 HIV-1 infected individuals on long-term ART, CCR5-edited cells constituted approximately 11-28% of the total circulating CD4⁺ T cells one-week post-infusion. Edited cell frequencies gradually declined, with an estimated half-life of 48 weeks, but persisted for up to 42 months. All participants experienced viral rebound approximately 2-4 weeks after starting ATI. A single grade 3 transfusion-related adverse event (fever, chills, or arthralgia) was observed, while the remaining adverse events were mild to moderate and transient. The presence of the characteristic five-nucleotide “pentamer” duplication at the ZFN target locus, detected by PCR-based assays, confirmed on-target editing with minimal off-target modifications [188]. A subsequent study evaluated ZFN-modified hematopoietic stem and progenitor cells (HSPCs) for sustained CCR5 disruption (NCT02500849) (Table 1) [189, 190]. Gene editing outcomes were verified using multiple orthogonal assays, including PCR amplification of the target site, surveyor nuclease mismatch detection, and targeted genome sequencing to confirm the disruption of CCR5 with high specificity. The editing efficiency ranged between 50-60% in the infused HSPC population. No severe or dose-limiting adverse events were reported; mild injection-site reactions and transient cytokine elevations (grade 1-2) resolved spontaneously. Depending on the cohort, follow-up ranged from 4 to 24 weeks. Viral rebound occurred at 2-4 weeks post-ATI, similar to that a in previous study.
The critical role of CCR5 in the HIV-1 life cycle and preclinical reports suggest that CCR5 antagonism can avert viral entry, which has led to the therapeutic development of strategies that can mutate CCR5 ex vivo, which can subsequently be administered to PLWH to achieve immune control and viral elimination [191-193]. In China, a clinical trial (NCT03164135) was conducted that recapitulated a similar clinical strategy that yielded a functional cure for HIV-1 in the London and Berlin patients. This trial employed CRISPR/Cas9-edited CCR5-ablated HSPCs that were transplanted into an HIV-1 infected individual with acute lymphoblastic leukemia (Table 1) [194]. The patient achieved complete donor chimerism, and long-term follow-up (~19 months) demonstrated stable engraftment of CCR5-disrupted cells (17.8% in vitro editing; 5.2-8.3% in vivo CCR5 disruption). Adverse events were limited to preconditioning-related toxicities, such as anemia, neutropenia, and thrombocytopenia. Viral rebound was observed approximately four weeks after ATI, prompting ART resumption. Gene disruption was confirmed by targeted deep sequencing, which demonstrated precise CRISPR-mediated cleavage with minimal off-target activity. The investigators concluded that the response of transplanted CD4+ T cells was insufficient for an HIV-1 cure but demonstrated that the long-term engraftment of CCR5-ablated HSPCs could sustain continuous peripheral cell production [194]. However, beyond technical challenges, ethical considerations add another layer of complexity to the widespread application of CCR5 editing [195].
Recently, a clinical trial of the investigational gene therapy EBT-101 (NCT05144386) evaluated a CRISPR-based dual-excision strategy delivered via an adeno-associated virus vector serotype 9 (AAV9) vector [196, 197]. This single ascending-dose, open-label study included six participants receiving stable ART. Treatment-emergent adverse events were predominantly grade 1 and 2 in severity, including transient complement activation, with no serious or dose-limiting toxicities. The median viral rebound occurred at 3-4 weeks post-ATI, although one participant maintained viral suppression for up to 16 weeks. The primary study follow-up is ongoing for 48 weeks, with long-term monitoring planned for up to 15 years to assess durability and safety. Viral reservoir changes were evaluated using an intact proviral DNA assay. The initial analysis found no evidence of off-target DNA cleavage, supporting the development of nucleic acid-based therapies for diverse populations. Another crucial strategy in the pursuit of a functional HIV-1 cure is the “shock-and-kill” approach, which was tested in a clinical study using LRAs to examine the combined effect of vorinostat with AGS-004 in five HIV-1 infected individuals on stable ART (NCT01069809) [188]. This study measured multiple parameters indicative of viral replication, including HIV-specific T cell responses and resting CD4+ T cell-associated viral RNA (rca-RNA) levels, after therapy. The goal was to combine vorinostat's latency reversal with HIV-specific immune induction through AGS-004; however, the therapeutic intervention had no significant impact on the pre-existing reservoir size, as assessed by a quantitative viral outgrowth assay (QVOA). Two out of five participants showed a decrease in rca-RNA, but this did not correlate with the infection levels in resting CD4+ T cells. The researchers attributed these results to the depletion of replication-incompetent cells and limited longitudinal data on rca-RNA [198]. Collectively, these early clinical investigations demonstrate that gene-editing strategies targeting CCR5 and integrated proviral DNA can be performed safely, with consistent in vivo persistence of edited cells and manageable adverse event profiles. However, the relatively short median time to viral rebound post-ATI underscores the need for higher engraftment efficiencies, more comprehensive reservoir targeting, including lymphoid tissues, and refined assays to confirm the longitudinal editing efficiency. Future studies integrating quantitative measures of engraftment, durability, and functional viral control are essential for advancing the translational potential of genome editing-based HIV-1 cure strategies (Figure 5).
5. Social and ethical considerations
Using stem cell transplantation in otherwise healthy individuals with well-controlled HIV infection on ART is ethically questionable because of the potential for graft-versus-host disease and transplant-related mortality, which together pose a significant risk [189]. Similarly, germline CCR5 editing in embryos has raised significant societal and regulatory concerns because of the potential for serious injury, disability, and misapplication if used without proper surveillance [199, 200]. For instance, in the first reported case of gene-edited babies, the scientist who used CRISPR-Cas9 to edit embryos was warned to conduct illegal medical procedures [201]. Recent ethical discussions have concluded that while safety remains the primary concern in debates over heritable genome editing, meaningful public engagement must also address deeper categorical and sociopolitical issues that reflect broader societal values [202, 203]. These issues highlight persistent barriers, including ethical dilemmas, safety risks, procedural challenges, and inadequate editing efficiency, which continue to hinder the widespread implementation of CCR5 editing strategies.
Recent discussions have emphasized that monotherapies are unlikely to provide lasting remission, increasing the interest in combination HIV cure strategies [204]. Approaches combining LRAs with immune-based interventions have strong preclinical and early clinical data but also raise additional safety and ethical issues [205-207]. Many LRAs, especially repurposed cancer drugs, have been linked to mutagenicity, off-target genetic effects, and blood-related toxicities, while their capacity to significantly reduce the latent reservoir remains unproven [206-208]. The participants in these studies warned that the widespread biological disruptions caused by latency reversal require personalized assessments, strict eligibility criteria, and long-term monitoring to minimize harm [206, 208]. Additionally, immune-based agents pose unique risks, making it difficult to ensure a favorable benefit-to-risk ratio for otherwise healthy individuals living with HIV [208, 209]. Another important factor is whether these strategies offer meaningful improvements over standard ART, which is safe, effective, and broadly accessible to patients. Stakeholders stressed that the expected benefits of any cure regimen must outweigh the risks and align with other priorities, such as reducing the treatment burden, enhancing the quality of life, and ensuring fair access [208]. Community involvement is crucial for defining relevant outcomes, managing expectations, and addressing stigma- and cost-related issues [208, 210]. Notably, structural barriers, such as limited industry incentives for collaboration and the absence of standardized trial endpoints, have been identified as obstacles to advancing combination HIV cure strategies [208]. Overall, both CCR5-targeted approaches and LRA immune-based combinations highlight the scientific and ethical challenges in advancing HIV cure research. To sustain trust and uphold ethical standards, clinical trial designs must include rigorous safety monitoring, early regulatory engagement, and continuous community input [205, 211]. Ultimately, balancing innovation with participant protection is crucial for transforming these investigational approaches into safe, scalable, and socially acceptable treatment options.
6. Conclusions and future perspectives
Targeting the HIV co-receptors CCR5 and CXCR4 and using lymphoid-targeting LNP approaches marks a major advancement in HIV therapy, especially in tackling the challenge of latent viral reservoirs [186]. While ART effectively suppresses HIV replication, these reservoirs are not eradicated, leading to viral rebound once treatment is stopped [186, 212].
Previous strategies, such as those using LRAs and bNAbs, have failed to eliminate reservoirs and have raised additional safety concerns, highlighting the need for more innovative solutions [213]. Next-generation CRISPR-Cas systems are promising tools for the precise editing of host co-receptors CCR5 and CXCR4, which are essential for HIV entry. These have shown potential in creating CD4+ T cells and HSCs resistant to both R5- and X4-tropic HIV strains, significantly decreasing viral reservoir sizes in infected animal models [38]. These results emphasize the therapeutic potential of co-receptor targeting to achieve sustained HIV suppression. However, the efficient delivery of CRISPR-Cas components remains a key challenge in therapeutic genome editing, with both viral and non-viral platforms actively explored for their potential to maximize editing efficiency while minimizing toxicity and off-target effects of treatment. Viral vectors, particularly AAV and lentiviruses, have been widely utilized because of their high transduction efficiency and ability to reach diverse cell types. AAV vectors are currently favored for in vivo applications because of their broad tissue tropism, low immunogenicity, and non-integrating nature, which contribute to their enhanced biosafety profiles [148, 158, 214]. However, the limited packaging capacity of AAVs (4.7-5.0 kb) limits their broad use when delivering large Cas9 systems with sgRNA [215], and pre-existing neutralizing antibodies can decrease transduction efficiency in humans [215, 216]. Lentiviral vectors enable stable gene integration and support delivery into non-dividing cells, with a high cargo capacity and the ability to target specific cell types through pseudotyping [181, 214, 217]. However, concerns regarding insertional mutagenesis have restricted their clinical use [181, 218]. Non-viral delivery systems, which are broadly categorized into physical and chemical approaches, offer modular and safer alternatives. Physical methods, such as electroporation, microinjection, and ultrasound-mediated delivery, facilitate direct cytosolic access but often damage cellular integrity, limiting their use to ex vivo and in vitro studies [219]. Chemical approaches, such as polymeric or lipid-based nanoparticles and liposomes, offer several advantages, including lower immunogenicity, reduced toxicity, and the ability to be surface-functionalized with targeting ligands for cell-specific delivery [184, 220-222]. Their cost-effectiveness, high cargo-loading capacity, and favorable biocompatibility make them promising candidates for next-generation gene delivery systems. However, challenges such as degradation during circulation, endosomal entrapment, and limited nuclear delivery in non-dividing cells must be addressed to fully realize their clinical potential [223, 224]. Ongoing research on advanced delivery platforms, rapid excision, and in situ mutation detection assays [146, 225] may further strengthen the efficacy and safety of these approaches by enabling real-time monitoring of genetic alterations in edited cells.
In summary, immune-based therapies, gene-editing technologies, and combinatorial approaches for viral elimination have shown promising outcomes in preclinical studies and are progressing through various stages of clinical evaluation. However, despite these advances, a definitive cure for HIV-1 remains elusive. Among these challenges, disruption of CXCR4 and CCR5 co-receptors through CRISPR-Cas9 editing presents potential long-term safety risks, including increased susceptibility to opportunistic infections, immune dysregulation, and impaired CAR-T cell trafficking. Therefore, a deeper understanding of HIV-1 pathogenesis, combined with careful management of safety concerns through optimized delivery systems and refined CRISPR technologies, would be essential for developing safer, more effective, and durable strategies toward a functional HIV-1 cure.
Abbreviations
AIDS: Acquired immunodeficiency syndrome; ARV: Antiretroviral; ART: Antiretroviral therapy; bNAbs: Broadly neutralizing antibodies; CAR T-cell: Chimeric antigen receptor T-cell; CRISPR: Clustered regularly interspaced short palindromic repeats; Cas9: CRISPR-associated protein 9; CCL5: C-C motif chemokine ligand 5; CCR5: C-C chemokine receptor type 5; CRS: Cytokine release syndrome; CTLA-4: Cytotoxic T-lymphocyte-associated protein 4; CXCL12: C-X-C chemokine ligand 12; CXCR4: C-X-C chemokine receptor type 4; CNS: Central nervous system; dCA: Didehydro-cortistatin A; HIV-1: Human immunodeficiency virus type 1; HSCs: Hematopoietic stem cells; HTLV-III: Human T-cell lymphotropic virus type III; iPSCs: Induced pluripotent stem cells; LASER-ART: Long-acting slow-effective release ART; LNs: Lymph nodes; LNPs: Lipid nanoparticles; LRAs: Latency-reversing agents; LTR: Long terminal repeat; MHC-I: Major histocompatibility complex class I; NIH: National institutes of health; PLWH: People living with HIV; PD-1: Programmed cell death protein 1; QVOA: Quantitative viral outgrowth assay; sgRNAs: Single-guide RNAs; SHIV: Simian-human immunodeficiency virus; SIV: Simian immunodeficiency virus; TALENs: Transcription activator-like effector nucleases; ULA ART: Ultra-long-acting antiretroviral therapy; Vpr: Viral protein R; ZFNs: Zinc-finger nucleases.
Acknowledgements
This study was supported by the University of Nebraska Foundation. Foundation support included research donations from Carol Swarts, M.D., Emerging Neuroscience Research Laboratory, and Margaret R. Larson Professorship. This research also received support from the National Institutes of Health grants 5R01MH121402, 1R01Al158160, R01 DA054535, PO1 DA028555, R01 NS126089, R01 NS36126, PO1 MH64570, P30 MH062261, 2R01 NS034239, and DP1-DA53719.
Competing interests
Dr. Howard Gendelman is a co-founder of Exavir Therapeutics, Inc., and NeuralRegen, Inc. Both are biotechnology companies. The former involves the development of ultra-long-acting drugs for chronic diseases, and the latter involves translating cellular regenerative therapies from the laboratory bench to the patient's bedside in neurodegenerative diseases. The viral elimination strategies, including the drugs and formulations described in this review, are not connected to those under development by either company. The other authors declare no conflicts of interest.
References
1. Control CfD, Prevention. Pneumocystis pneumonia-Los Angeles. 1981. MMWR Morbidity and mortality weekly report. 1996;45:729-33
2. Barré-Sinoussi F, Chermann J-C, Rey F, Nugeyre MT, Chamaret S, Gruest J. et al. Isolation of a T-lymphotropic retrovirus from a patient at risk for acquired immune deficiency syndrome (AIDS). Science. 1983;220:868-71
3. Gallo RC, Salahuddin SZ, Popovic M, Shearer GM, Kaplan M, Haynes BF. et al. Frequent detection and isolation of cytopathic retroviruses (HTLV-III) from patients with AIDS and at risk for AIDS. science. 1984;224:500-3
4. Coffin J, Haase A, Levy JA, Montagnier L, Oroszlan S, Teich N. et al. Human immunodeficiency viruses. Science. 1986;232:697
5. Wain-Hobson S, Vartanian J-P, Henry M, Chenciner N, Cheynier R, Delassus S. et al. LAV revisited: origins of the early HIV-1 isolates from Institut Pasteur. Science. 1991;252:961-5
6. Ratner L, Haseltine W, Patarca R, Livak KJ, Starcich B, Josephs SF. et al. Complete nucleotide sequence of the AIDS virus, HTLV-III. Nature. 1985;313:277-84
7. Shaw GM, Hahn BH, Arya SK, Groopman JE, Gallo RC, Wong-Staal F. Molecular characterization of human T-cell leukemia (lymphotropic) virus type III in the acquired immune deficiency syndrome. Science. 1984;226:1165-71
8. Gonda MA. Molecular genetics and structure of the human immunodeficiency virus. Journal of electron microscopy technique. 1988;8:17-40
9. Van Heuvel Y, Schatz S, Rosengarten JF, Stitz J. Infectious RNA: Human immunodeficiency virus (HIV) biology, therapeutic intervention, and the quest for a vaccine. Toxins. 2022;14:138
10. Frankel AD, Young JA. HIV-1: fifteen proteins and an RNA. Annual review of biochemistry. 1998;67:1-25
11. Miller RH, Sarver N. HIV accessory proteins: emerging therapeutic targets. Molecular medicine. 1995;1:479-85
12. Faust TB, Binning JM, Gross JD, Frankel AD. Making sense of multifunctional proteins: human immunodeficiency virus type 1 accessory and regulatory proteins and connections to transcription. Annual Review of Virology. 2017;4:241-60
13. Wilen CB, Tilton JC, Doms RW. HIV: cell binding and entry. Cold Spring Harbor perspectives in medicine. 2012;2:a006866
14. Melikyan GB. Common principles and intermediates of viral protein-mediated fusion: the HIV-1 paradigm. Retrovirology. 2008;5:111
15. Hu W-S, Hughes SH. HIV-1 reverse transcription. Cold Spring Harbor perspectives in medicine. 2012;2:a006882
16. Engelman A, Cherepanov P. The structural biology of HIV-1: mechanistic and therapeutic insights. Nature Reviews Microbiology. 2012;10:279-90
17. Chen B. Molecular mechanism of HIV-1 entry. Trends in microbiology. 2019;27:878-91
18. Freed EO. HIV-1 assembly, release and maturation. Nature reviews microbiology. 2015;13:484-96
19. Chen J, Zhou T, Zhang Y, Luo S, Chen H, Chen D. et al. The reservoir of latent HIV. Frontiers in cellular and infection microbiology. 2022;12:945956
20. McMyn NF, Varriale J, Fray EJ, Zitzmann C, MacLeod H, Lai J. et al. The latent reservoir of inducible, infectious HIV-1 does not decrease despite decades of antiretroviral therapy. The Journal of clinical investigation. 2023 133
21. Chun T-W, Justement JS, Murray D, Hallahan CW, Maenza J, Collier AC. et al. Rebound of plasma viremia following cessation of antiretroviral therapy despite profoundly low levels of HIV reservoir: implications for eradication. Aids. 2010;24:2803-8
22. Coffin JM, Hughes SH. Clonal expansion of infected CD4+ T cells in people living with HIV. Viruses. 2021;13:2078
23. Sengupta S, Siliciano RF. Targeting the latent reservoir for HIV-1. Immunity. 2018;48:872-95
24. Chun T-W, Moir S, Fauci AS. HIV reservoirs as obstacles and opportunities for an HIV cure. Nature immunology. 2015;16:584-9
25. Cohn LB, Chomont N, Deeks SG. The biology of the HIV-1 latent reservoir and implications for cure strategies. Cell host & microbe. 2020;27:519-30
26. Zhu L, Huang B, Wang X, Ni F, Ao M, Wang R. et al. Highly potent and broadly neutralizing anti-CD4 trimeric nanobodies inhibit HIV-1 infection by inducing CD4 conformational alteration. Nature Communications. 2024;15:6961
27. Dragic T, Litwin V, Allaway GP, Martin SR, Huang Y, Nagashima KA. et al. HIV-1 entry into CD4+ cells is mediated by the chemokine receptor CC-CKR-5. Nature. 1996;381:667-73
28. Feng Y, Broder CC, Kennedy PE, Berger EA. HIV-1 entry cofactor: functional cDNA cloning of a seven-transmembrane, G protein-coupled receptor. Science. 1996;272:872-7
29. Moore JP, Trkola A, Dragic T. Co-receptors for HIV-1 entry. Current opinion in immunology. 1997;9:551-62
30. Zhang Z, Zhang H, Zheng L, Chen S, Du S, Xiao J. et al. CXCR4 mediated recognition of HIV envelope spike and inhibition by CXCL12. Nature Communications. 2025;16:8653
31. Singh P, Mohammad KS, Pelus LM. CXCR4 expression in the bone marrow microenvironment is required for hematopoietic stem and progenitor cell maintenance and early hematopoietic regeneration after myeloablation. Stem Cells. 2020;38:849-59
32. Chong SZ, Evrard M, Devi S, Chen J, Lim JY, See P. et al. CXCR4 identifies transitional bone marrow premonocytes that replenish the mature monocyte pool for peripheral responses. Journal of experimental medicine. 2016;213:2293-314
33. Werner Y, Mass E, Ashok Kumar P, Ulas T, Händler K, Horne A. et al. Cxcr4 distinguishes HSC-derived monocytes from microglia and reveals monocyte immune responses to experimental stroke. Nature neuroscience. 2020;23:351-62
34. Herrera C, Sanchez J, Torres A, Pascual A, Rueda A, Alvarez MA. Pattern of expression of CXCR4 and adhesion molecules by human CD34+ cells from different sources: role in homing efficiency in NOD/SCID mice. Haematologica. 2004;89:1037-45
35. Wu L, Paxton WA, Kassam N, Ruffing N, Rottman JB, Sullivan N. et al. CCR5 levels and expression pattern correlate with infectability by macrophage-tropic HIV-1, in vitro. The Journal of experimental medicine. 1997;185:1681-92
36. Spano J-P, Andre F, Morat L, Sabatier L, Besse B, Combadiere C. et al. Chemokine receptor CXCR4 and early-stage non-small cell lung cancer: pattern of expression and correlation with outcome. Annals of Oncology. 2004;15:613-7
37. Giovannetti Ensoli, Mazzetta Cristofaro D, Pierdominici Muratori. et al. CCR5 and CXCR4 chemokine receptor expression and β-chemokine production during early T cell repopulation induced by highly active anti-retroviral therapy. Clinical & Experimental Immunology. 1999;118:87-94
38. Li S, Holguin L, Burnett JC. CRISPR-Cas9-mediated gene disruption of HIV-1 co-receptors confers broad resistance to infection in human T cells and humanized mice. Molecular Therapy Methods & Clinical Development. 2022;24:321-31
39. Knipping F, Newby GA, Eide CR, McElroy AN, Nielsen SC, Smith K. et al. Disruption of HIV-1 co-receptors CCR5 and CXCR4 in primary human T cells and hematopoietic stem and progenitor cells using base editing. Molecular therapy. 2022;30:130-44
40. Bleul CC, Wu L, Hoxie JA, Springer TA, Mackay CR. The HIV coreceptors CXCR4 and CCR5 are differentially expressed and regulated on human T lymphocytes. Proceedings of the National Academy of Sciences. 1997;94:1925-30
41. Dean M, Carrington M, Winkler C, Huttley GA, Smith MW, Allikmets R. et al. Genetic restriction of HIV-1 infection and progression to AIDS by a deletion allele of the CKR5 structural gene. Science. 1996;273:1856-62
42. Kitchen SG, Zack JA. CXCR4 expression during lymphopoiesis: implications for human immunodeficiency virus type 1 infection of the thymus. Journal of virology. 1997;71:6928-34
43. Connell BJ, Hermans LE, Wensing AM, Schellens I, Schipper PJ, van Ham PM. et al. Immune activation correlates with and predicts CXCR4 co-receptor tropism switch in HIV-1 infection. Scientific reports. 2020;10:15866
44. Dorr P, Westby M, Dobbs S, Griffin P, Irvine B, Macartney M. et al. Maraviroc (UK-427,857), a potent, orally bioavailable, and selective small-molecule inhibitor of chemokine receptor CCR5 with broad-spectrum anti-human immunodeficiency virus type 1 activity. Antimicrobial agents and chemotherapy. 2005;49:4721-32
45. Jähnichen S, Blanchetot C, Maussang D, Gonzalez-Pajuelo M, Chow KY, Bosch L. et al. CXCR4 nanobodies (VHH-based single variable domains) potently inhibit chemotaxis and HIV-1 replication and mobilize stem cells. Proceedings of the National Academy of Sciences. 2010;107:20565-70
46. Hütter G, Nowak D, Mossner M, Ganepola S, Müßig A, Allers K. et al. Long-term control of HIV by CCR5 Delta32/Delta32 stem-cell transplantation. New England Journal of Medicine. 2009;360:692-8
47. Sankaranantham M. HIV-Is a cure possible? Indian journal of sexually transmitted diseases and AIDS. 2019;40:1-5
48. Henrich TJ, Hanhauser E, Hu Z, Stellbrink H-J, Noah C, Martin JN. et al. Viremic control and viral coreceptor usage in two HIV-1-infected persons homozygous for CCR5 Δ32. Aids. 2015;29:867-76
49. Henrich TJ, Hu Z, Li JZ, Sciaranghella G, Busch MP, Keating SM. et al. Long-term reduction in peripheral blood HIV type 1 reservoirs following reduced-intensity conditioning allogeneic stem cell transplantation. The Journal of infectious diseases. 2013;207:1694-702
50. Manotham K, Chattong S, Setpakdee A. Generation of CCR5-defective CD34 cells from ZFN-driven stop codon-integrated mesenchymal stem cell clones. Journal of Biomedical Science. 2015;22:25
51. Armani-Tourret M, Bone B, Tan TS, Sun W, Bellefroid M, Struyve T. et al. Immune targeting of HIV-1 reservoir cells: a path to elimination strategies and cure. Nature Reviews Microbiology. 2024;22:328-44
52. Jones JE, Le Sage V, Lakdawala SS. Viral and host heterogeneity and their effects on the viral life cycle. Nature Reviews Microbiology. 2021;19:272-82
53. Harper J, Betts MR, Lichterfeld M, Müller-Trutwin M, Margolis D, Bar KJ. et al. Progress note 2024: curing HIV; not in my lifetime or just around the corner? Pathogens and Immunity. 2024;8:115
54. Matsuda K, Maeda K. HIV reservoirs and treatment strategies toward curing HIV infection. International Journal of Molecular Sciences. 2024;25:2621
55. Chou TC, Maggirwar NS, Marsden MD. HIV persistence, latency, and cure approaches: where are we now? Viruses. 2024;16:1163
56. Bouabida K, Chaves BG, Anane E. Challenges and barriers to HIV care engagement and care cascade. Frontiers in reproductive health. 2023;5:1201087
57. Natarajan K, Dimasi N, Wang J, Mariuzza RA, Margulies DH. Structure and function of natural killer cell receptors: multiple molecular solutions to self, nonself discrimination. Annual review of immunology. 2002;20:853-85
58. Wherry EJ, Kurachi M. Molecular and cellular insights into T cell exhaustion. Nature reviews immunology. 2015;15:486-99
59. Foka FET, Mufhandu HT. Current ARTs, virologic failure, and implications for AIDS management: a systematic review. Viruses. 2023;15:1732
60. Chawla A, Wang C, Patton C, Murray M, Punekar Y, de Ruiter A. et al. A review of long-term toxicity of antiretroviral treatment regimens and implications for an aging population. Infectious diseases and therapy. 2018;7:183-95
61. Fridman I, Ubel PA, Blumenthal-Barby J, England CV, Currier JS, Eyal N. et al. “Cure” versus “clinical remission”: the impact of a medication description on the willingness of people living with HIV to take a medication. AIDS and Behavior. 2020;24:2054-61
62. Deeks SG, Lewin SR, Ross AL, Ananworanich J, Benkirane M, Cannon P. et al. International AIDS Society global scientific strategy: towards an HIV cure 2016. Nature medicine. 2016;22:839-50
63. Spivak AM, Planelles V. HIV-1 eradication: early trials (and tribulations). Trends in molecular medicine. 2016;22:10-27
64. Towards an HIV cure. a global scientific strategy. Nature reviews Immunology. 2012;12:607-14
65. Xu W, Li H, Wang Q, Hua C, Zhang H, Li W. et al. Advancements in developing strategies for sterilizing and functional HIV cures. BioMed research international. 2017;2017:6096134
66. Henderson LJ, Reoma LB, Kovacs JA, Nath A. Advances toward curing HIV-1 infection in tissue reservoirs. Journal of virology. 2020;94:10.1128 /jvi. 00375-19
67. Ma X, Yang T, Luo Y, Wu L, Jiang Y, Song Z. et al. TRIM28 promotes HIV-1 latency by SUMOylating CDK9 and inhibiting P-TEFb. Elife. 2019;8:e42426
68. Abner E, Jordan A. HIV "shock and kill" therapy: In need of revision. Antiviral Res. 2019;166:19-34
69. Ait-Ammar A, Kula A, Darcis G, Verdikt R, De Wit S, Gautier V. et al. Current Status of Latency Reversing Agents Facing the Heterogeneity of HIV-1 Cellular and Tissue Reservoirs. Front Microbiol. 2019;10:3060
70. Rodari A, Darcis G, Van Lint CM. The Current Status of Latency Reversing Agents for HIV-1 Remission. Annu Rev Virol. 2021;8:491-514
71. Hong X, Schouest B, Xu H. Effects of exosome on the activation of CD4+ T cells in rhesus macaques: a potential application for HIV latency reactivation. Scientific reports. 2017;7:15611
72. Tang X, Lu H, Dooner M, Chapman S, Quesenberry PJ, Ramratnam B. Exosomal Tat protein activates latent HIV-1 in primary, resting CD4+ T lymphocytes. JCI insight. 2018;3:e95676
73. Klinnert S, Schenkel CD, Freitag PC, Günthard HF, Plückthun A, Metzner KJ. Targeted shock-and-kill HIV-1 gene therapy approach combining CRISPR activation, suicide gene tBid and retargeted adenovirus delivery. Gene Ther. 2024;31:74-84
74. Copertino DC Jr, Holmberg CS, Weiler J, Ward AR, Howard JN, Levinger C. et al. The latency-reversing agent HODHBt synergizes with IL-15 to enhance cytotoxic function of HIV-specific T cells. JCI Insight. 2023 8
75. Kim JT, Zhang TH, Carmona C, Lee B, Seet CS, Kostelny M. et al. Latency reversal plus natural killer cells diminish HIV reservoir in vivo. Nat Commun. 2022;13:121
76. Dashti A, Sukkestad S, Horner AM, Neja M, Siddiqi Z, Waller C. et al. AZD5582 plus SIV-specific antibodies reduce lymph node viral reservoirs in antiretroviral therapy-suppressed macaques. Nat Med. 2023;29:2535-46
77. Cao S, Slack SD, Levy CN, Hughes SM, Jiang Y, Yogodzinski C. et al. Hybrid nanocarriers incorporating mechanistically distinct drugs for lymphatic CD4(+) T cell activation and HIV-1 latency reversal. Sci Adv. 2019;5:eaav6322
78. Wu L, Zheng Z, Xun J, Liu L, Wang J, Zhang X. et al. Anti-PD-L1 antibody ASC22 in combination with a histone deacetylase inhibitor chidamide as a "shock and kill" strategy for ART-free virological control: a phase II single-arm study. Signal Transduct Target Ther. 2024;9:231
79. Gruell H, Gunst JD, Cohen YZ, Pahus MH, Malin JJ, Platten M. et al. Effect of 3BNC117 and romidepsin on the HIV-1 reservoir in people taking suppressive antiretroviral therapy (ROADMAP): a randomised, open-label, phase 2A trial. Lancet Microbe. 2022;3:e203-e14
80. Chew GM, Fujita T, Webb GM, Burwitz BJ, Wu HL, Reed JS. et al. TIGIT marks exhausted T cells, correlates with disease progression, and serves as a target for immune restoration in HIV and SIV infection. PLoS pathogens. 2016;12:e1005349
81. Hoffmann M, Pantazis N, Martin GE, Hickling S, Hurst J, Meyerowitz J. et al. Exhaustion of activated CD8 T cells predicts disease progression in primary HIV-1 infection. PLoS pathogens. 2016;12:e1005661
82. Moron-Lopez S, Kim P, Søgaard OS, Tolstrup M, Wong JK, Yukl SA. Characterization of the HIV-1 transcription profile after romidepsin administration in ART-suppressed individuals. Aids. 2019;33:425-31
83. Klinnert S, Schenkel CD, Freitag PC, Günthard HF, Plückthun A, Metzner KJ. Targeted shock-and-kill HIV-1 gene therapy approach combining CRISPR activation, suicide gene tBid and retargeted adenovirus delivery. Gene Therapy. 2024;31:74-84
84. Ahlenstiel CL, Symonds G, Kent SJ, Kelleher AD. Block and lock HIV cure strategies to control the latent reservoir. Frontiers in cellular and infection microbiology. 2020;10:424
85. Debyser Z, Vansant G, Bruggemans A, Janssens J, Christ F. Insight in HIV integration site selection provides a block-and-lock strategy for a functional cure of HIV infection. Viruses. 2018;11:12
86. Shrivastava S, Ray RM, Holguin L, Echavarria L, Grepo N, Scott TA. et al. Exosome-mediated stable epigenetic repression of HIV-1. Nature communications. 2021;12:5541
87. Kessing CF, Nixon CC, Li C, Tsai P, Takata H, Mousseau G. et al. In vivo suppression of HIV rebound by didehydro-cortistatin A, a “block-and-lock” strategy for HIV-1 treatment. Cell reports. 2017;21:600-11
88. Mousseau G, Kessing CF, Fromentin R, Trautmann L, Chomont N, Valente ST. The Tat inhibitor didehydro-cortistatin A prevents HIV-1 reactivation from latency. MBio. 2015;6:10.1128 /mbio. 00465-15
89. Méndez C, Ledger S, Petoumenos K, Ahlenstiel C, Kelleher AD. RNA-induced epigenetic silencing inhibits HIV-1 reactivation from latency. Retrovirology. 2018;15:67
90. Moranguinho I, Valente ST. Block-and-lock: new horizons for a cure for HIV-1. Viruses. 2020;12:1443
91. Li C, Mori L, Valente ST. The block-and-lock strategy for human immunodeficiency virus cure: lessons learned from didehydro-cortistatin A. The Journal of Infectious Diseases. 2021;223:S46-S53
92. Vargas B, Sluis-Cremer N. Toward a functional cure for HIV-1 infection: the block and lock therapeutic approach. Frontiers in Virology. 2022;2:917941
93. Vansant G, Bruggemans A, Janssens J, Debyser Z. Block-and-lock strategies to cure HIV infection. Viruses. 2020;12:84
94. Chen Z, Julg B. Therapeutic vaccines for the treatment of HIV. Translational Research. 2020;223:61-75
95. Day CL, Kaufmann DE, Kiepiela P, Brown JA, Moodley ES, Reddy S. et al. PD-1 expression on HIV-specific T cells is associated with T-cell exhaustion and disease progression. Nature. 2006;443:350-4
96. Trautmann L, Janbazian L, Chomont N, Said EA, Gimmig S, Bessette B. et al. Upregulation of PD-1 expression on HIV-specific CD8+ T cells leads to reversible immune dysfunction. Nature medicine. 2006;12:1198-202
97. Borthwick N, Fernandez N, Hayes PJ, Wee EG, Yildirim BMA, Baines A, et al. Safety and immunogenicity of the ChAdOx1-MVA-vectored conserved mosaic HIVconsvX candidate T-cell vaccines in HIV-CORE 005.2, an open-label, dose-escalation, first-in-human, phase 1 trial in adults living without HIV-1 in the UK. The Lancet Microbe. 2025; 6
98. Li S, Moog C, Zhang T, Su B. HIV reservoir: antiviral immune responses and immune interventions for curing HIV infection. Chinese Medical Journal. 2022;135:2667-76
99. Caskey M. Broadly neutralizing antibodies for the treatment and prevention of HIV infection. Current Opinion in HIV and AIDS. 2020;15:49-55
100. Gautam R, Nishimura Y, Gaughan N, Gazumyan A, Schoofs T, Buckler-White A. et al. A single injection of crystallizable fragment domain-modified antibodies elicits durable protection from SHIV infection. Nature medicine. 2018;24:610-6
101. Shingai M, Donau OK, Plishka RJ, Buckler-White A, Mascola JR, Nabel GJ. et al. Passive transfer of modest titers of potent and broadly neutralizing anti-HIV monoclonal antibodies block SHIV infection in macaques. Journal of Experimental Medicine. 2014;211:2061-74
102. Julg B, Liu P-T, Wagh K, Fischer WM, Abbink P, Mercado NB. et al. Protection against a mixed SHIV challenge by a broadly neutralizing antibody cocktail. Science translational medicine. 2017;9:eaao4235
103. Shingai M, Nishimura Y, Klein F, Mouquet H, Donau OK, Plishka R. et al. Antibody-mediated immunotherapy of macaques chronically infected with SHIV suppresses viraemia. Nature. 2013;503:277-80
104. Wu Y, Xue J, Wang C, Li W, Wang L, Chen W. et al. Rapid elimination of broadly neutralizing antibodies correlates with treatment failure in the acute phase of simian-human immunodeficiency virus infection. Journal of Virology. 2019;93:10.1128 /jvi. 01077-19
105. Halper-Stromberg A, Lu C-L, Klein F, Horwitz JA, Bournazos S, Nogueira L. et al. Broadly neutralizing antibodies and viral inducers decrease rebound from HIV-1 latent reservoirs in humanized mice. Cell. 2014;158:989-99
106. Borducchi EN, Liu J, Nkolola JP, Cadena AM, Yu W-H, Fischinger S. et al. Antibody and TLR7 agonist delay viral rebound in SHIV-infected monkeys. Nature. 2018;563:360-4
107. Lim S-Y, Lee J, Osuna CE, Vikhe P, Schalk DR, Chen E. et al. Induction of durable remission by dual immunotherapy in SHIV-infected ART-suppressed macaques. Science. 2024;383:1104-11
108. Gunst JD, Højen JF, Pahus MH, Rosás-Umbert M, Stiksrud B, McMahon JH. et al. Impact of a TLR9 agonist and broadly neutralizing antibodies on HIV-1 persistence: the randomized phase 2a TITAN trial. Nature medicine. 2023;29:2547-58
109. Karuna S, Laher F, Dadabhai S, Yu PC, Grove D, Orrell C. et al. Analytical treatment interruption among women with HIV in southern Africa who received VRC01 or placebo in the Antibody Mediated Prevention Study: ATI stakeholder engagement, implementation and early clinical data. Journal of the International AIDS Society. 2025;28:e26495
110. Julg B, Walker-Sperling VE, Wagh K, Aid M, Stephenson KE, Zash R. et al. Safety and antiviral effect of a triple combination of HIV-1 broadly neutralizing antibodies: a phase 1/2a trial. Nature Medicine. 2024;30:3534-43
111. Dingens AS, Arenz D, Weight H, Overbaugh J, Bloom JD. An antigenic atlas of HIV-1 escape from broadly neutralizing antibodies distinguishes functional and structural epitopes. Immunity. 2019;50:520-32 e3
112. Qi J, Ding C, Jiang X, Gao Y. Advances in developing CAR T-cell therapy for HIV cure. Frontiers in Immunology. 2020;11:361
113. Walker RE, Bechtel CM, Natarajan V, Baseler M, Hege KM, Metcalf JA. et al. Long-term in vivo survival of receptor-modified syngeneic T cells in patients with human immunodeficiency virus infection. Blood, The Journal of the American Society of Hematology. 2000;96:467-74
114. Ali A, Kitchen SG, Chen IS, Ng HL, Zack JA, Yang OO. HIV-1-specific chimeric antigen receptors based on broadly neutralizing antibodies. Journal of virology. 2016;90:6999-7006
115. Liu B, Zou F, Lu L, Chen C, He D, Zhang X. et al. Chimeric antigen receptor T cells guided by the single-chain Fv of a broadly neutralizing antibody specifically and effectively eradicate virus reactivated from latency in CD4+ T lymphocytes isolated from HIV-1-infected individuals receiving suppressive combined antiretroviral therapy. Journal of virology. 2016;90:9712-24
116. Urak RZ, Soemardy C, Ray R, Li S, Shevchenko G, Scott T. et al. Conditionally replicating vectors mobilize chimeric antigen receptors against HIV. Molecular Therapy Methods & Clinical Development. 2020;19:285-94
117. Zhen A, Carrillo MA, Mu W, Rezek V, Martin H, Hamid P. et al. Robust CAR-T memory formation and function via hematopoietic stem cell delivery. PLoS pathogens. 2021;17:e1009404
118. Maldini CR, Gayout K, Leibman RS, Dopkin DL, Mills JP, Shan X. et al. HIV-resistant and HIV-specific CAR-modified CD4+ T cells mitigate HIV disease progression and confer CD4+ T cell help in vivo. Molecular Therapy. 2020;28:1585-99
119. Maldini CR, Claiborne DT, Okawa K, Chen T, Dopkin DL, Shan X. et al. Dual CD4-based CAR T cells with distinct costimulatory domains mitigate HIV pathogenesis in vivo. Nature medicine. 2020;26:1776-87
120. Zhen A, Peterson CW, Carrillo MA, Reddy SS, Youn CS, Lam BB. et al. Long-term persistence and function of hematopoietic stem cell-derived chimeric antigen receptor T cells in a nonhuman primate model of HIV/AIDS. PLoS pathogens. 2017;13:e1006753
121. Barber-Axthelm IM, Barber-Axthelm V, Sze KY, Zhen A, Suryawanshi GW, Chen IS. et al. Stem cell-derived CAR T cells traffic to HIV reservoirs in macaques. JCI insight. 2021;6:e141502
122. Liu B, Zhang W, Xia B, Jing S, Du Y, Zou F. et al. Broadly neutralizing antibody-derived CAR T cells reduce viral reservoir in individuals infected with HIV-1. The Journal of clinical investigation. 2021 131
123. Zhen A, Carrillo MA, Kitchen SG. Chimeric antigen receptor engineered stem cells: a novel HIV therapy. Immunotherapy. 2017;9:401-10
124. Campos-Gonzalez G, Martinez-Picado J, Velasco-Hernandez T, Salgado M. Opportunities for CAR-T cell immunotherapy in HIV cure. Viruses. 2023;15:789
125. Wherry EJ. T cell exhaustion. Nature immunology. 2011;12:492-9
126. Le Garff G, Samri A, Lambert-Niclot S, Even S, Lavolé A, Cadranel J. et al. Transient HIV-specific T cells increase and inflammation in an HIV-infected patient treated with nivolumab. Aids. 2017;31:1048-51
127. Saibil S, Ohashi P. Targeting T cell activation in immuno-oncology. Current Oncology. 2020;27:S98
128. Buck AM, Deveau T-M, Henrich TJ, Deitchman AN. Challenges in HIV-1 latent reservoir and target cell quantification in CAR-T cell and other lentiviral gene modifying HIV cure strategies. Viruses. 2023;15:1126
129. Bailon L, Mothe B, Berman L, Brander C. Novel approaches towards a functional cure of HIV/AIDS. Drugs. 2020;80:859-68
130. Borrajo A. Breaking barriers to an HIV-1 cure: innovations in gene editing, immune modulation, and reservoir eradication. Life. 2025;15:276
131. Rothemejer FH, Lauritsen NP, Søgaard OS, Tolstrup M. Strategies for enhancing CAR T cell expansion and persistence in HIV infection. Frontiers in Immunology. 2023;14:1253395
132. York J, Gowrishankar K, Micklethwaite K, Palmer S, Cunningham AL, Nasr N. Evolving strategies to eliminate the CD4 T cells HIV viral reservoir via CAR T cell immunotherapy. Frontiers in Immunology. 2022;13:873701
133. Ollerton MT, Berger EA, Connick E, Burton GF. HIV-1-specific chimeric antigen receptor T cells fail to recognize and eliminate the follicular dendritic cell HIV reservoir in vitro. Journal of Virology. 2020;94:10.1128 /jvi. 00190-20
134. Rothemejer FH, Lauritsen NP, Juhl AK, Schleimann MH, König S, Søgaard OS. et al. Development of HIV-resistant CAR T cells by CRISPR/Cas-mediated CAR integration into the CCR5 locus. Viruses. 2023;15:202
135. Doudna JA, Charpentier E. The new frontier of genome engineering with CRISPR-Cas9. Science. 2014;346:1258096
136. Gaj T, Gersbach CA, Barbas CF. ZFN, TALEN, and CRISPR/Cas-based methods for genome engineering. Trends in biotechnology. 2013;31:397-405
137. Barrangou R, Doudna JA. Applications of CRISPR technologies in research and beyond. Nature biotechnology. 2016;34:933-41
138. Hodge CA, Donegan NP, Armstrong DA, Hayden MS, Howell AL. Enhanced cleavage of genomic CCR5 using CASX2Max. RNA biology. 2025;22:1-18
139. Kim Y-G, Chandrasegaran S. Chimeric restriction endonuclease. Proceedings of the National Academy of Sciences. 1994;91:883-7
140. Kim Y-G, Cha J, Chandrasegaran S. Hybrid restriction enzymes: zinc finger fusions to Fok I cleavage domain. Proceedings of the National Academy of Sciences. 1996;93:1156-60
141. Porteus MH, Carroll D. Gene targeting using zinc finger nucleases. Nature biotechnology. 2005;23:967-73
142. Wilen CB, Wang J, Tilton JC, Miller JC, Kim KA, Rebar EJ. et al. Engineering HIV-resistant human CD4+ T cells with CXCR4-specific zinc-finger nucleases. PLoS pathogens. 2011;7:e1002020
143. Yuan J, Wang J, Crain K, Fearns C, Kim KA, Hua KL. et al. Zinc-finger nuclease editing of human cxcr4 promotes HIV-1 CD4+ T cell resistance and enrichment. Molecular Therapy. 2012;20:849-59
144. Benjamin R, Berges BK, Solis-Leal A, Igbinedion O, Strong CL, Schiller MR. TALEN gene editing takes aim on HIV. Human genetics. 2016;135:1059-70
145. Romito M, Juillerat A, Kok YL, Hildenbeutel M, Rhiel M, Andrieux G. et al. Preclinical evaluation of a novel TALEN targeting CCR5 confirms efficacy and safety in conferring resistance to HIV-1 infection. Biotechnology journal. 2021;16:2000023
146. Zhao M, Wen J, Chen IS, Liu J, Lu Y. Excision of HIV-1 Provirus in Human Primary Cells with Nanocapsuled TALEN Proteins. ACS applied bio materials. 2025;8:1227-39
147. Jinek M, Chylinski K, Fonfara I, Hauer M, Doudna JA, Charpentier E. A programmable dual-RNA-guided DNA endonuclease in adaptive bacterial immunity. science. 2012;337:816-21
148. Dash PK, Chen C, Kaminski R, Su H, Mancuso P, Sillman B. et al. CRISPR editing of CCR5 and HIV-1 facilitates viral elimination in antiretroviral drug-suppressed virus-infected humanized mice. Proceedings of the National Academy of Sciences. 2023;120:e2217887120
149. Wilbie D, Walther J, Mastrobattista E. Delivery aspects of CRISPR/Cas for in vivo genome editing. Accounts of chemical research. 2019;52:1555-64
150. Ali MU, Chaudhary BN, Panja S, Gendelman HE. Theranostic Diagnostics. Intercellular and Interorganellar Transfer and Communication in Biology and Medicine. 2024:551-78
151. Saayman S, Ali SA, Morris KV, Weinberg MS. The therapeutic application of CRISPR/Cas9 technologies for HIV. Expert opinion on biological therapy. 2015;15:819-30
152. Ebina H, Misawa N, Kanemura Y, Koyanagi Y. Harnessing the CRISPR/Cas9 system to disrupt latent HIV-1 provirus. Scientific reports. 2013;3:2510
153. Zhang M, Lang Y, Li W. Multiplexed CRISPR-Cas system targeting ASFV genes in vivo: solution lies within. Microbiology Spectrum. 2024;12:e00714-24
154. Zhang C, Li H, Bidasee KR, Gendelman HE, Dash PK. Therapeutic Gene Editing. Neuroimmune Pharmacology and Therapeutics: Springer. 2024 p. 1005-24
155. Gurrola TE, Effah SN, Sariyer IK, Dampier W, Nonnemacher MR, Wigdahl B. Delivering CRISPR to the HIV-1 reservoirs. Frontiers in microbiology. 2024;15:1393974
156. Mohamed H, Gurrola T, Berman R, Collins M, Sariyer IK, Nonnemacher MR. et al. Targeting CCR5 as a component of an HIV-1 therapeutic strategy. Frontiers in immunology. 2022;12:816515
157. Hu W, Kaminski R, Yang F, Zhang Y, Cosentino L, Li F. et al. RNA-directed gene editing specifically eradicates latent and prevents new HIV-1 infection. Proceedings of the National Academy of Sciences. 2014;111:11461-6
158. Dash PK, Kaminski R, Bella R, Su H, Mathews S, Ahooyi TM. et al. Sequential LASER ART and CRISPR treatments eliminate HIV-1 in a subset of infected humanized mice. Nature communications. 2019;10:2753
159. Hou P, Chen S, Wang S, Yu X, Chen Y, Jiang M. et al. Genome editing of CXCR4 by CRISPR/cas9 confers cells resistant to HIV-1 infection. Scientific reports. 2015;5:15577
160. Tebas P, Jadlowsky JK, Shaw PA, Tian L, Esparza E, Brennan AL. et al. CCR5-edited CD4+ T cells augment HIV-specific immunity to enable post-rebound control of HIV replication. The Journal of clinical investigation. 2024 131
161. Wang W, Ye C, Liu J, Zhang D, Kimata JT, Zhou P. CCR5 gene disruption via lentiviral vectors expressing Cas9 and single guided RNA renders cells resistant to HIV-1 infection. PloS one. 2014;9:e115987
162. Li C, Guan X, Du T, Jin W, Wu B, Liu Y. et al. Inhibition of HIV-1 infection of primary CD4+ T-cells by gene editing of CCR5 using adenovirus-delivered CRISPR/Cas9. Journal of General Virology. 2015;96:2381-93
163. Kang H, Minder P, Park MA, Mesquitta W-T, Torbett BE, Slukvin II. CCR5 disruption in induced pluripotent stem cells using CRISPR/Cas9 provides selective resistance of immune cells to CCR5-tropic HIV-1 virus. Molecular therapy Nucleic acids. 2015 4
164. Yu S, Yao Y, Xiao H, Li J, Liu Q, Yang Y. et al. Simultaneous knockout of CXCR4 and CCR5 genes in CD4+ T cells via CRISPR/Cas9 confers resistance to both X4-and R5-tropic human immunodeficiency virus type 1 infection. Human gene therapy. 2018;29:51-67
165. Liu Z, Chen S, Jin X, Wang Q, Yang K, Li C. et al. Genome editing of the HIV co-receptors CCR5 and CXCR4 by CRISPR-Cas9 protects CD4+ T cells from HIV-1 infection. Cell & bioscience. 2017;7:47
166. Xiao Q, Guo D, Chen S. Application of CRISPR/Cas9-based gene editing in HIV-1/AIDS therapy. Frontiers in cellular and infection microbiology. 2019;9:69
167. Bhowmik R, Chaubey B. CRISPR/Cas9: a tool to eradicate HIV-1. AIDS Research and Therapy. 2022;19:58
168. Li T, Yang Y, Qi H, Cui W, Zhang L, Fu X. et al. CRISPR/Cas9 therapeutics: progress and prospects. Signal transduction and targeted therapy. 2023;8:36
169. Xu L, Yang H, Gao Y, Chen Z, Xie L, Liu Y. et al. CRISPR/Cas9-mediated CCR5 ablation in human hematopoietic stem/progenitor cells confers HIV-1 resistance in vivo. Molecular Therapy. 2017;25:1782-9
170. Claiborne DT, Detwiler Z, Docken SS, Borland TD, Cromer D, Simkhovich A. et al. High frequency CCR5 editing in human hematopoietic stem progenitor cells protects xenograft mice from HIV infection. Nature communications. 2025;16:446
171. Sharma M, Afrin F, Satija N, Tripathi RP, Gangenahalli GU. Stromal-derived factor-1/CXCR4 signaling: indispensable role in homing and engraftment of hematopoietic stem cells in bone marrow. Stem cells and development. 2011;20:933-46
172. Luther SA, Cyster JG. Chemokines as regulators of T cell differentiation. Nature immunology. 2001;2:102-7
173. González-Arriagada WA, García IE, Martínez-Flores R, Morales-Pison S, Coletta RD. Therapeutic perspectives of HIV-associated chemokine receptor (CCR5 and CXCR4) antagonists in carcinomas. International Journal of Molecular Sciences. 2022;24:478
174. Chaudary N, Pintilie M, Jelveh S, Lindsay P, Hill RP, Milosevic M. Plerixafor improves primary tumor response and reduces metastases in cervical cancer treated with radio-chemotherapy. Clinical Cancer Research. 2017;23:1242-9
175. Halvorsen EC, Hamilton MJ, Young A, Wadsworth BJ, LePard NE, Lee H-N. et al. Maraviroc decreases CCL8-mediated migration of CCR5+ regulatory T cells and reduces metastatic tumor growth in the lungs. Oncoimmunology. 2016;5:e1150398
176. Jiao X, Nawab O, Patel T, Kossenkov AV, Halama N, Jaeger D. et al. Recent advances targeting CCR5 for cancer and its role in immuno-oncology. Cancer research. 2019;79:4801-7
177. Alum EU, Uti DE, Ugwu OP-C, Alum BN. Toward a cure-Advancing HIV/AIDs treatment modalities beyond antiretroviral therapy: A Review. Medicine. 2024;103:e38768
178. Moso MA, Roche M, Cevaal PM, Lewin SR. CRISPR/Cas9 for achieving postintervention HIV control. Current Opinion in HIV and AIDS. 2025;20:432-40
179. Chaudhary BN, Ali MU, Gendelman HE. Theranostics for Viral Infections. Neuroimmune Pharmacology and Therapeutics: Springer. 2024 p. 617-37
180. Herskovitz J, Hasan M, Patel M, Kevadiya BD, Gendelman HE. Pathways toward a functional HIV-1 cure: Balancing promise and perils of CRISPR therapy. HIV Reservoirs: Methods and Protocols. 2022:429-45
181. Herskovitz J, Hasan M, Patel M, Blomberg WR, Cohen JD, Machhi J. et al. CRISPR-Cas9 mediated exonic disruption for HIV-1 elimination. EBioMedicine. 2021 73
182. Khamaikawin W, Saisawang C, Tassaneetrithep B, Bhukhai K, Phanthong P, Borwornpinyo S. et al. CRISPR/Cas9 genome editing of CCR5 combined with C46 HIV-1 fusion inhibitor for cellular resistant to R5 and X4 tropic HIV-1. Scientific reports. 2024;14:10852
183. Patel M, Panja S, Zaman LA, Yeapuri P, Bhattarai S, Gorantla S. et al. CCR5-ligand decorated rilpivirine lipid-based nanoparticles for sustained antiretroviral responses. Nature communications. 2025;16:513
184. Panja S, Zaman LA, Zhang C, Patel M, Gorantla S, Dash PK. et al. Lymphoid and CXCR4 Cell Targeted Lipid Nanoparticles Facilitate HIV-1 Proviral DNA Excision. Advanced Healthcare Materials. 2025: 2501190.
185. Liu S, Wang Q, Yu X, Li Y, Guo Y, Liu Z. et al. HIV-1 inhibition in cells with CXCR4 mutant genome created by CRISPR-Cas9 and piggyBac recombinant technologies. Scientific Reports. 2018;8:1-11
186. Wang J-W, Liu J-H, Xun J-J. CCR5 gene editing and HIV immunotherapy: current understandings, challenges, and future directions. Frontiers in Immunology. 2025;16:1590690
187. Cillo AR, Mellors JW. Which therapeutic strategy will achieve a cure for HIV-1? Current opinion in virology. 2016;18:14-9
188. Tebas P, Stein D, Tang WW, Frank I, Wang SQ, Lee G. et al. Gene editing of CCR5 in autologous CD4 T cells of persons infected with HIV. New England Journal of Medicine. 2014;370:901-10
189. Karuppusamy KV, Babu P, Thangavel S. The strategies and challenges of CCR5 gene editing in hematopoietic stem and progenitor cells for the treatment of HIV. Stem Cell Reviews and Reports. 2021;17:1607-18
190. DiGiusto DL, Cannon PM, Holmes MC, Li L, Rao A, Wang J. et al. Preclinical development and qualification of ZFN-mediated CCR5 disruption in human hematopoietic stem/progenitor cells. Molecular therapy Methods & clinical development. 2016 3
191. Wilkin TJ, Gulick RM. CCR5 antagonism in HIV infection: current concepts and future opportunities. Annual review of medicine. 2012;63:81-93
192. Ding J, Liu Y, Lai Y. Knowledge from London and Berlin: finding threads to a functional HIV cure. Frontiers in Immunology. 2021;12:688747
193. Gupta RK, Peppa D, Hill AL, Gálvez C, Salgado M, Pace M. et al. Evidence for HIV-1 cure after CCR5Δ32/Δ32 allogeneic haemopoietic stem-cell transplantation 30 months post analytical treatment interruption: a case report. The Lancet HIV. 2020;7:e340-e7
194. Xu L, Wang J, Liu Y, Xie L, Su B, Mou D. et al. CRISPR-edited stem cells in a patient with HIV and acute lymphocytic leukemia. New England Journal of Medicine. 2019;381:1240-7
195. Kanazawa J, Gianella S, Concha-Garcia S, Taylor J, Kaytes A, Christensen C. et al. Ethical and practical considerations for HIV cure-related research at the end-of-life: a qualitative interview and focus group study in the United States. BMC medical ethics. 2022;23:2
196. Presti R, Kennedy W, Craddick T, Gordon J. First-in-Human study of EBT-101 in aviremic HIV-1 infected adults on stable ART. Proceedings of the 27th Annual Meeting of the American Society of Gene & Cell Therapy. 2024
197. BioTherapeutics. E. Study of EBT-101 in Aviremic HIV-1 Infected Adults on Stable ART. ClinicalTrialsgov. 2024
198. Gay CL, Kuruc JD, Falcinelli SD, Warren JA, Reifeis SA, Kirchherr JL. et al. Assessing the impact of AGS-004, a dendritic cell-based immunotherapy, and vorinostat on persistent HIV-1 Infection. Scientific Reports. 2020;10:5134
199. Xu M. CCR5-Δ32 biology, gene editing, and warnings for the future of CRISPR-Cas9 as a human and humane gene editing tool. Cell & bioscience. 2020;10:48
200. Niemiec E, Howard HC. Ethical issues related to research on genome editing in human embryos. Computational and structural biotechnology journal. 2020;18:887-96
201. Cyranoski D. The CRISPR-baby scandal: what's next for human gene-editing. Nature. 2019;566:440-3
202. Almeida M, Ranisch R. Beyond safety: mapping the ethical debate on heritable genome editing interventions. Humanities and Social Sciences Communications. 2022;9:1-14
203. Hayenhjelm M, Nordlund C. Consequence Arguments for and Against Germline Editing. The Risks and Ethics of Human Gene Editing: A Philosophical Guide to the Arguments: Springer. 2025 p. 117-51
204. Deeks SG, Archin N, Cannon P, Collins S, Jones RB, de Jong MA. et al. Research priorities for an HIV cure: international AIDS society global scientific strategy 2021. Nature medicine. 2021;27:2085-98
205. Sciences CfIOoM. International ethical guidelines for health-related research involving humans: Prepared by the Council for International Organizations of Medical Sciences (CIOMS) in collaboration with the World Health Organization (WHO): Council for International Organizations of Medical Sciences; 2016
206. Tioka L, Diez RC, Sönnerborg A, van de Klundert MA. Latency Reversing Agents and the Road to an HIV Cure. Pathogens. 2025;14:232
207. Debrabander Q, Hensley KS, Psomas CK, Bramer W, Mahmoudi T, Van Welzen BJ. et al. The efficacy and tolerability of latency-reversing agents in reactivating the HIV-1 reservoir in clinical studies: a systematic review. Journal of virus eradication. 2023;9:100342
208. Dubé K, Kanazawa J, Dee L, Taylor J, Sauceda JA, Gianella S. et al. Considerations for designing and implementing combination HIV cure trials: findings from a qualitative in-depth interview study in the United States. AIDS Research and Therapy. 2021;18:75
209. Kanazawa J, Gianella S, Concha-Garcia S, Taylor J, Kaytes A, Christensen C. et al. Ethical and practical considerations for interventional HIV cure-related research at the end-of-life: a qualitative study with key stakeholders in the United States. PLoS One. 2021;16:e0254148
210. Joint United Nations Programme on HIV/AIDS and the World Health Organization. Ethical considerations in HIV prevention trials. Geneva. 2021
211. HANC. Recommendations for Community Engagement in HIV/AIDS Research; 2020
212. Zhang C, Li H, Poluektova LY, Gendelman HE, Dash PK. Unique molecular signatures in rebound viruses from antiretroviral drug and CRISPR-treated HIV-1-infected humanized mice. Communications Biology. 2025;8:1077
213. Zhang C, Zaman LA, Poluektova LY, Gorantla S, Gendelman HE, Dash PK. Humanized mice for studies of HIV-1 persistence and elimination. Pathogens. 2023;12:879
214. Bella R, Kaminski R, Mancuso P, Young W-B, Chen C, Sariyer R. et al. Removal of HIV DNA by CRISPR from patient blood engrafts in humanized mice. Molecular Therapy Nucleic Acids. 2018;12:275-82
215. Benatti HR, Gray-Edwards HL. Adeno-associated virus delivery limitations for neurological indications. Mary Ann Liebert, Inc, publishers 140 Huguenot Street, 3rd Floor New …. 2022 p. 1-7
216. S. Selot R, Hareendran S, R. Jayandharan G. Developing immunologically inert adeno-associated virus (AAV) vectors for gene therapy: possibilities and limitations. Current pharmaceutical biotechnology. 2013;14:1072-82
217. Arduini A, Katiyar H, Liang C. Progress in Pseudotyping Lentiviral Vectors Towards Cell-Specific Gene Delivery In Vivo. Viruses. 2025;17:802
218. Yew C-HT, Gurumoorthy N, Nordin F, Tye GJ, Zaman WSWK, Tan JJ. et al. Integrase deficient lentiviral vector: prospects for safe clinical applications. PeerJ. 2022;10:e13704
219. Lino CA, Harper JC, Carney JP, Timlin JA. Delivering CRISPR: a review of the challenges and approaches. Drug delivery. 2018;25:1234-57
220. Wang L, Wang G, Mao W, Chen Y, Rahman MM, Zhu C. et al. Bioinspired engineering of fusogen and targeting moiety equipped nanovesicles. Nature Communications. 2023;14:3366
221. Wang H-X, Song Z, Lao Y-H, Xu X, Gong J, Cheng D. et al. Nonviral gene editing via CRISPR/Cas9 delivery by membrane-disruptive and endosomolytic helical polypeptide. Proceedings of the National Academy of Sciences. 2018;115:4903-8
222. Demirci S, Essawi K, Germino-Watnick P, Liu X, Hakami W, Tisdale JF. Advances in CRISPR delivery methods: perspectives and challenges. The CRISPR Journal. 2022;5:660-76
223. Chen Y, Ping Y. Development of CRISPR/Cas delivery systems for in vivo precision genome editing. Accounts of Chemical Research. 2023;56:2185-96
224. Li K, Zhang Q. Eliminating the HIV tissue reservoir: current strategies and challenges. Infectious Diseases. 2024;56:165-82
225. Rahman MM, Wang L, Chen Y, Rahman MM, Al Islam MO, Lee LP. et al. Rapid in situ mutation detection in extracellular vesicle DNA. Extracellular Vesicles and Circulating Nucleic Acids. 2025;6:72
226. Gay CL, James KS, Tuyishime M, Falcinelli SD, Joseph SB, Moeser MJ. et al. Stable latent HIV infection and low-level viremia despite treatment with the broadly neutralizing antibody VRC07-523LS and the latency reversal agent vorinostat. The Journal of Infectious Diseases. 2022;225:856-61
227. da Costa LC, Bomfim LM, Dittz UVT, Velozo CdA, da Cunha RD, Tanuri A. Repression of HIV-1 reactivation mediated by CRISPR/dCas9-KRAB in lymphoid and myeloid cell models. Retrovirology. 2022;19:12
Author contact
![]() Corresponding authors: Dr. Howard E. Gendelman (Phone: 402-559-8920; Email: hegendeledu; Fax: 402-559-7495) and Dr. Sudipta Panja (Email: sudipta.panjaedu).
Corresponding authors: Dr. Howard E. Gendelman (Phone: 402-559-8920; Email: hegendeledu; Fax: 402-559-7495) and Dr. Sudipta Panja (Email: sudipta.panjaedu).
 Global reach, higher impact
Global reach, higher impact